Types of Glaucoma Surgery for Glaucoma Treatment.
Glaucoma manifests as a collection of disorders united by a progressive damage to the optic nerve. This damage leads to a distinct optic disc appearance and an identifiable pattern of irreversible visual field impairments. While frequently connected with heightened intraocular pressure (IOP), this link is neither universal nor exclusive.
Hence, while IOP remains a prominent risk factor, it’s not the sole precursor to glaucoma. The term ‘ocular hypertension’ characterizes cases marked by consistently elevated IOP without concurrent glaucomatous harm. Conversely, the designation ‘normal’ or ‘low tension glaucoma’ (NTG/LTG) describes the characteristic optic disc cupping and visual field defects seen alongside a normal or low IOP.
Types of glaucoma
In terms of clinical and etiological aspects, glaucoma assumes various forms:
A. Congenital/Developmental Glaucomas
- Primary Congenital Glaucoma: Occurs without associated anomalies.
- Developmental Glaucoma: Presents with concurrent anomalies.
B. Primary Adult Glaucomas
- Primary Open-Angle Glaucomas (POAG): Predominant among adult cases, characterized by open anterior chamber angles.
- Primary Angle-Closure Glaucoma (PACG): Features closure of the anterior chamber angle.
- Primary Mixed Mechanism Glaucoma: Exhibits combined attributes of both open-angle and angle-closure mechanisms.
C. Secondary Glaucomas: Arises due to underlying conditions or factors such as trauma, uveitis, or steroid use, which contribute to the elevation of intraocular pressure.
Understanding this intricate classification not only aids in accurate diagnosis but also guides the selection of appropriate management strategies, reflecting the dynamic nature of glaucoma as a complex and multifaceted ocular challenge.
Info on Timolol eye drops for glaucoma.
Types of Glaucoma Surgery
1. PERIPHERAL IRIDECTOMY

Indications
- Treatment of all stages of primary angle-closure glaucoma.
- Prophylaxis in the fellow eye.
Note. Laser iridotomy should always be preferred over surgical iridectomy.
2. GONIOTOMY AND TRABECULOTOMY
These operations are indicated in congenital and developmental glaucomas
Goniotomy
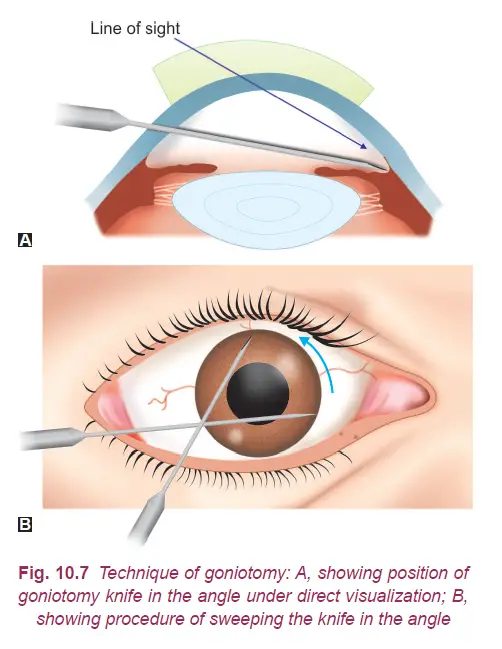
Goniotomy is a procedure where a Barkan’s goniotomy knife is introduced through the limbus on the temporal side. With gonioscopic guidance, the knife is threaded across the anterior chamber to the nasal angle. An incision is created in the angle, approximately halfway between the iris root and Schwalbe’s ring, spanning around 75 degrees. The knife is then withdrawn. While the process might need to be repeated, the success rate eventually reaches around 85%.
Trabeculotomy
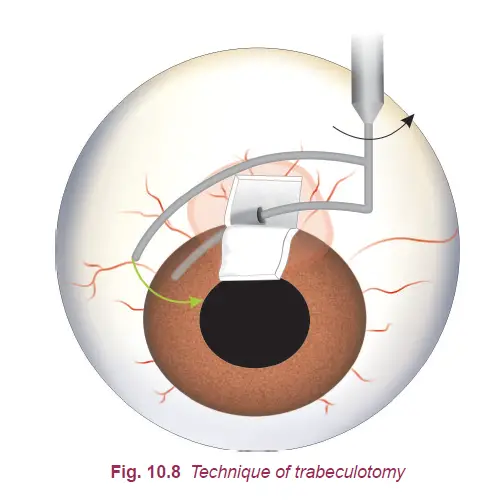
Trabeculotomy is beneficial when clouding of the cornea obstructs angle visualization or if goniotomy has proved ineffective. During this technique, a vertical scleral incision is made at around 12 o’clock position after creating a conjunctival flap and partial-thickness scleral flap. Harm’s trabeculotome’s lower prong is navigated along Schlemm’s canal on one side, guided by the upper prong. The trabeculotome is rotated to disrupt the inner wall over a quarter of the canal. This process is repeated on the opposite side. The key challenge here lies in accurately locating Schlemm’s canal.
FILTERING OPERATIONS
Filtering operations serve to establish a fresh route for the drainage of aqueous humor, effectively managing intraocular pressure (IOP) to levels below 21 mm Hg. These operations can be categorized as follows:
A. External filteration surgery
- Free-filtering operations (Full thickness fistula). These are no longer performed nowadays, because of high rate of postoperative complications.Their names are mentioned only for historical interest. These operations included Elliot’s sclerocorneal trephining, punch sclerectomy, Scheie’s thermosclerostomy and iridencleisis.
- Guarded filtering surgery (Partial thickness fistula e.g., trabeculectomy).
- Non-penetrating filtration surgery e.g., deep sclerectomy and viscocanalostomy.
B. Internal filteration surgery
- Primary angle-closure glaucoma with peripheral anterior synechial involving more than 270° angle
or where PI and medical treatment fail. - Primary open-angle glaucoma not controlled with medical treatment.
- Congenital and developmental glaucomas where trabeculotomy and goniotomy fail.
- Secondary glaucomas where medical therapy is not effective.
A. External Filtration Surgery
Trabeculectomy, first introduced by Carain in 1980, stands as the most commonly performed surgery for partial thickness filtration to this day.
Indications:
- Primary Angle-Closure Glaucoma: When peripheral anterior synechiae involve more than a 270° angle or when peripheral iridotomy and medical interventions prove unsuccessful.
- Primary Open-Angle Glaucoma: If the condition remains unmanageable through medical approaches.
- Congenital and Developmental Glaucomas: After trabeculotomy and goniotomy have proven ineffective.
- Secondary Glaucomas: In instances where medical treatment falls short in effectiveness.
Non-Penetrating Filtration Surgeries
In response to concerns over postoperative complications such as endophthalmitis, overfiltration, and hypotony, non-penetrating filtration surgeries have gained attention. These procedures avoid entering the anterior chamber. However, they typically result in less effective intraocular pressure (IOP) control compared to traditional trabeculectomy. Currently, two main techniques are utilized:
- Deep Sclerectomy: This approach involves creating a partial-thickness scleral flap, similar to conventional trabeculectomy. A second deep partial-thickness scleral flap is then formed and removed, leaving a delicate membrane consisting of thin sclera, trabeculum, and Descemet’s membrane. This membrane facilitates the diffusion of aqueous humor. The upper scleral flap is gently repositioned, and the conjunctival incision is closed.
- Viscocanalostomy: Similar to deep sclerectomy, this method involves excising the deeper scleral flap. However, a high-viscosity viscoelastic substance is injected into Schlemm’s canal using a specialized cannula.
While non-penetrating filtration surgeries address certain postoperative complications, they often trade off with inferior IOP control in comparison to conventional trabeculectomy.
B.Internal Filtration Surgeries
Internal filtration surgeries, often referred to as canal-based procedures, represent more recent techniques aimed at reestablishing filtration via Schlemm’s canal. These procedures are designed to maintain natural anatomy and eliminate the need for a conjunctival bleb, thereby reducing the risk of long-term endophthalmitis and ocular hypotony. Notable procedures in this category include:
- Canaloplasty: Involves dilation and circumferential traction of the canal using a 10–0 prolene suture.
- Trabectome: Utilizes an ab interno microcautery to ablate the trabecular meshwork and inner wall of Schlemm’s canal.
- iStent: A titanium micro device implanted within Schlemm’s canal, enabling direct flow of aqueous humor into the canal, bypassing the trabecular meshwork.
Glaucoma Drainage Device Operations
Glaucoma drainage devices, also referred to as glaucoma valve implants, are plastic devices designed to facilitate the drainage of aqueous humor. These devices establish a connection between the anterior chamber of the eye and the sub-Tenon’s space. The surgical procedure involving the use of a glaucoma valve implant is commonly known as a Seton operation.
The glaucoma drainage devices frequently utilized include Molteno, Krupin-Denver, and Ahmed glaucoma valve (AGV).
Indications of artificial drainage shunts encompass:
- Neovascular glaucoma,
- Glaucoma associated with aniridia,
- Cases of primary and secondary glaucoma that remain refractory even after trabeculectomy with adjunct antimetabolite therapy has proven ineffective.
Cyclo-Destructive Procedures
Cyclo-destructive procedures are employed to lower intraocular pressure (IOP) by targeting and damaging segments of the ciliary epithelium responsible for aqueous humor secretion. This reduction in secretion subsequently contributes to lowered IOP levels.
Indications: These procedures find primary utility in cases of absolute glaucomas.
The cyclo-destructive procedures currently practiced encompass:
- Cyclocryotherapy
- Nd: Yag Laser Cyclodestruction
- Diode Laser Cyclophotocoagulation
Laser Treatments for Glaucoma:
In the realm of glaucoma management, laser treatments have emerged as valuable interventions to address intraocular pressure and its associated complications. This article delves into various laser surgical options available to patients, shedding light on their mechanisms, applications, and efficacy.
Argon Laser Trabeculoplasty (ALT): An ingenious technique, ALT effectively alleviates clogs within the eye, facilitating the drainage of excess fluid. Its success rate, around 75%, proves particularly beneficial for the most prevalent form of glaucoma. In a staged approach, treatment may be initiated on a portion of the clogs, followed by the remaining ones later.
Selective Laser Trabeculoplasty (SLT): For cases where ALT might fall short, SLT steps in with its precision-focused approach. Targeting specific pressure points with a low-level laser, SLT offers a gradual, customizable treatment. Often employed as the primary surgical method due to its specificity.
Laser Peripheral Iridotomy (LPI): Addressing the challenges of narrow-angle glaucoma, LPI employs a laser beam to create a minute aperture in the iris. This procedure facilitates drainage, releasing accumulated fluid and alleviating pressure between the iris and cornea.
Cyclophotocoagulation: When conventional treatments prove inadequate, cyclophotocoagulation enters the scene. By directing a laser into the eye’s internal structures, it eases intraocular pressure. While requiring periodic repetition, this method becomes a viable option when fluid buildup remains unmanageable through other approaches.
When to have Glaucoma Surgery
When facing the challenges of glaucoma, medical interventions are often the initial line of defense. Prescription eye drops or, in rare cases, oral medications are commonly employed to regulate intraocular pressure. However, when pharmaceutical treatments prove inadequate, the role of surgery becomes paramount.
Progression to Surgical Solutions: Surgical intervention becomes a viable path when medicinal approaches fail to effectively manage intraocular pressure. It marks a crucial transition point in glaucoma treatment, ensuring that the condition’s progression is adequately addressed.
Considering Surgical Options: In instances where prescription medications result in severe side effects such as heightened blood pressure, rapid heartbeat, or impotence, the prospect of surgery gains prominence. The potential benefits of surgical intervention extend beyond pressure control, providing an alternative for those who cannot tolerate medication-related side effects.
Urgency of Surgical Action: In certain cases, the urgency for surgical intervention is evident. Individuals with notably high eye pressure that jeopardizes their vision might require immediate surgical measures to mitigate the risks to their eyesight. In such scenarios, surgery serves as a rapid and essential countermeasure.
As the threshold between medical and surgical management, the decision to proceed with surgery should be guided by comprehensive medical evaluation, consultation with eye care professionals, and a thorough understanding of individual circumstances.
Reference : (AK Khurana)
Choosing the Best Smart Thermostat
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.