Diabetic retinopathy (DR) encompasses retinal alterations observed in individuals with diabetes mellitus. As the life expectancy of diabetic patients rises, the prevalence of diabetic retinopathy has surged. Regrettably, diabetic retinopathy stands as a prominent contributor to visual impairment and blindness.
Also see: Updated criteria for Legal blindness in America.
Diabetic Retinopathy symptoms
Diabetic retinopathy, a potentially serious ocular complication of diabetes mellitus, can often remain asymptomatic during its nonproliferative stages. This subtlety makes it possible for the condition to silently progress without causing noticeable symptoms. This phenomenon is rooted in the fact that blood vessels don’t consistently leak during these initial stages, which underscores the importance of regular eye examinations for early detection.
The Silent Progression: Nonproliferative Stages
During the nonproliferative stages of diabetic retinopathy, individuals often experience a lack of symptoms. This absence of apparent warning signs can mask the presence of the condition, leading to its stealthy progression. This is attributed to the fact that blood vessels in the retina may not be actively leaking or causing significant visual disturbances during this phase.
The Turning Point: Proliferative Diabetic Retinopathy
As diabetic retinopathy advances to the proliferative stage, symptoms may begin to emerge, serving as potential indicators of the escalating condition. It is at this juncture that the condition becomes more noticeable and warrants attention. Proliferative diabetic retinopathy is characterized by the proliferation of abnormal blood vessels, and the associated symptoms can include:
- Increased Number of Eye Floaters: Individuals may perceive an uptick in the presence of eye floaters. These are tiny specks or threads that drift across the field of vision.
- Blurry Vision: Blurred vision can manifest as a result of fluid leakage or bleeding into the retina. This can impact the clarity of visual perception.
- Distorted Vision: Visual distortions, such as straight lines appearing wavy or bent, can occur due to the structural changes within the retina caused by the abnormal blood vessels.
- Poor Night Vision: Impaired ability to see clearly in low-light conditions, particularly during nighttime, can be indicative of proliferative diabetic retinopathy.
- Loss of Vision: In severe cases, the proliferation of abnormal blood vessels can lead to significant visual impairment or even vision loss.
- Decreased Field of Vision: The field of vision may become compromised, with individuals experiencing limitations in their peripheral or central visual fields.
- Change in Colors: Some individuals may notice alterations in how they perceive colors, which can be attributed to the impact of proliferative diabetic retinopathy on retinal function.
The Significance of Early Detection
While symptoms may become apparent during the proliferative stage, it’s important to note that diabetic retinopathy can be detected in its earlier, non-symptomatic stages through comprehensive eye examinations conducted by qualified eye care specialists or ophthalmologists. These evaluations play a pivotal role in identifying the condition before symptoms emerge, offering a window of opportunity for timely intervention and management.
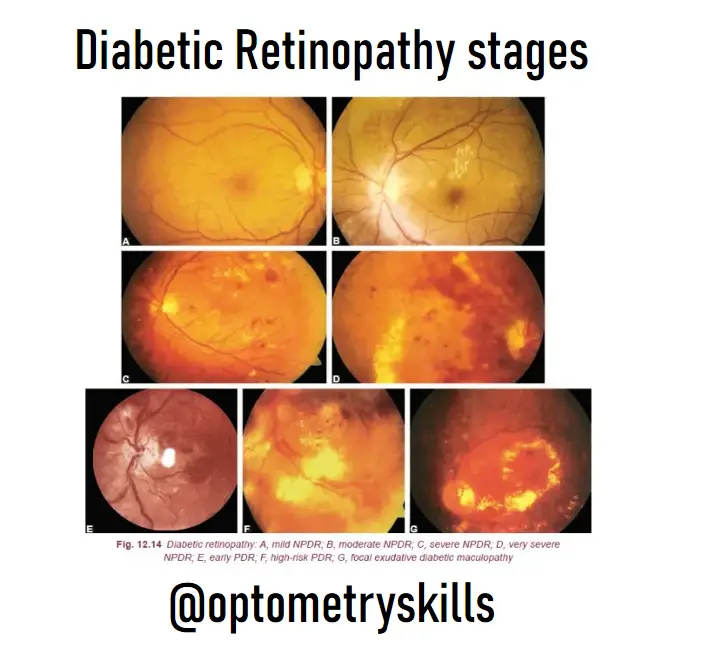
Diabetic Retinopathy stages
The duration of diabetes stands as a pivotal determinant in the progression of diabetic retinopathy.
- Beyond a span of 10 years, approximately 20% of individuals with type I diabetes and 25% with type II diabetes manifest signs of retinopathy.
- Extending to 20 years, the prevalence escalates, encompassing around 90% of type I diabetics and 60% of type II diabetics with retinopathy.
- Crossing the threshold of 30 years, an overwhelming 95% of both type I and type II diabetics exhibit retinopathy.
Classification of Diabetic Retinopathy types
Diabetic retinopathy has been variously classified. Presently followed classification is as follows:
I. Non-proliferative diabetic retinopathy (NPDR)
- Mild NPDR
- Moderate NPDR
- Severe NPDR
- Very severe NPDR
II. Proliferative diabetic retinopathy (PDR)
III. Diabetic maculopathy
IV. Advanced diabetic eye disease (ADED)
Diabetic Retinopathy stages

ETDRS study classification: On the basis of severity of the above findings the NPDR has been further classified as under:
- Mild NPDR
- At least one microaneurysm must be present.
- Moderate NPDR
- Microaneurysms/intraretinal haemorrhage in
2 or 3 quadrants. - Early mild IRMA.
- Hard/soft exudates may or may not present.
- Severe NPDR. Any one of the following (4–2–1 Rule)
- Four quadrants of microaneurysms and
extensive intraretinal haemorrhages. - Two quadrants of venous beading.
- One quadrant of IRMA changes.
- Very severe NPDR. Any two of the following (4–2–1 Rule)
- Four quadrants of microaneurysms and
extensive intraretinal haemorrhages. - Two quadrants of venous beading.
- One quadrant of IRMA changes.
II. Proliferative diabetic retinopathy (PDR) Proliferative diabetic retinopathy develops in more than 50% of cases after about 25 years of the onset of disease. Therefore, it is more
common in patients with juvenile onset diabetes.
On the basis of high-risk characteristics (HRCs) described by diabetic retinopathy study (DRS) group, the PDR can be further classified as below:
- Early NVD or NVE PDR without HRCs (Early PDR)and
- PDR with HRCs. High-risk characteristics (HRC) of PDR are as follows
- NVD 1/4 to 1/3 of disc area with or without vitreous haemorrhage (VH) or preretinal haemorrhage (PRH)
- NVD <1/4 disc area with VH or PRH
- NVE >1/2 disc area with VH or PRH
Prevention of Diabetic Retinopathy
The journey towards preventing diabetic retinopathy commences with the meticulous management of blood sugar levels—a cornerstone for preserving the health of the eyes.
Mastering Blood Sugar Management
Effective prevention of diabetic retinopathy hinges on the art of managing diabetes itself. This intricate practice encompasses a trifecta of elements: judicious medication, well-balanced dietary choices, and a regimen of consistent physical activity. A pivotal step involves vigilant monitoring of blood sugar levels, a practice that empowers individuals to remain informed about their metabolic state. Should the challenge of maintaining optimal levels arise, consulting a healthcare professional becomes paramount.
Nourishing Your Body: The Role of Diet
Crafting a diet that fuels your well-being is pivotal in the battle against diabetic retinopathy. A nourishing dietary regimen embraces elements that are intrinsically diabetes-friendly:
- Low Glycemic Carbohydrates: Incorporating carbohydrates with a low glycemic index helps regulate blood sugar levels effectively.
- Abundant Vegetables and Fruits: Loading your plate with vibrant vegetables and fruits provides essential nutrients that contribute to overall health.
- Wholesome Whole Grains: Opting for whole grains rather than refined alternatives offers a sustained energy release, fostering steady blood sugar levels.
- Nutrient-Rich Legumes: Legumes, enriched with fiber and protein, contribute to balanced blood sugar levels.
- Nourishing Dairy: Low-fat dairy options supply essential nutrients without inducing spikes in blood sugar.
- Healthy Fats: Embracing the goodness of healthy fats found in avocados and nuts not only supports overall health but also aids in diabetes management.
- Heart-Healthy Fish: Introducing heart-healthy fish, such as salmon and tuna, into your diet further enriches your nutritional arsenal.
The Multi-Faceted Approach to Diabetes Management
Diabetic retinopathy prevention extends beyond blood sugar management. Controlling blood pressure and cholesterol levels assumes pivotal importance in safeguarding ocular health. A proactive stance against tobacco consumption contributes to the comprehensive strategy aimed at preventing diabetic retinopathy.
Diabetic retinopathy checkup routine
To prevent visual loss occurring from diabetic retinopathy a periodic follow-up is very important for a timely intervention. The recommendations for periodic fundus examination are as follows:
- First examination, 5 years after diagnosis of
type 1 DM and at the time of diagnosis in type 2 DM. - Every year, till there is no diabetic retinopathy or
there is mild NPDR. - Every 6 months, in moderate NPDR.
- Every 3 months, in severe NPDR.
- Every 2 months, in PDR with no high-risk characteristics.
Treatment options for Diabetic Retinopathy
Various treatment modalities are employed to tackle the multifaceted aspects of this condition, ranging from metabolic control to advanced surgical interventions.
Metabolic Control and Risk Factor Management
The foundation of diabetic retinopathy management lies in achieving and maintaining metabolic control of diabetes mellitus (DM) along with addressing associated risk factors. Stable blood glucose levels are crucial, with fasting levels ideally below 120 mg% and post-prandial levels below 180 mg%.
Another critical marker, HbA1c (glycosylated haemoglobin), should be maintained below 7%. Dyslipidemia control is equally important, with targets including fasting cholesterol levels below 200 mg%, triglycerides under 150 mg%, HDL above 50 mg%, and LDL below 150 mg%. Monitoring renal function is essential, with recommended targets of serum creatinine at 1.0 mg%, blood urea at 20–40 mg%, and 24-hour urinary protein below 200 mg%.
Managing associated anemia (target hemoglobin >10 mg%) and hypertension (target blood pressure of 130/80 mm Hg) further contribute to comprehensive management. Lifestyle changes such as smoking cessation, alcohol avoidance, and regular exercise are emphasized.
Intravitreal Anti-VEGF Drugs
Vascular endothelial growth factor (VEGF) plays a central role in the development of diabetic retinopathy. Intravitreal anti-VEGF drugs such as Bevacizumab and Ranibizumab have emerged as potent therapeutic options.
Administered intravitrealy in small volumes, these drugs lead to significant improvements in vision and stabilization of visual acuity in a substantial percentage of cases. The role of these agents in inhibiting VEGF’s pathological effects is pivotal, rendering them a cornerstone in contemporary management.
Intravitreal Steroids and Laser Therapy
Intravitreal steroids, particularly triamcinolone acetonide (IVTA), also contribute to the therapeutic armamentarium. IVTA restores the inner retinal barrier and exhibits some anti-VEGF effects. However, potential complications such as glaucoma, cataract formation, and susceptibility to endophthalmitis limit its use.
Laser therapy, on the other hand, employs the principles of stimulating the retinal pigment epithelium (RPE) pump mechanism and inhibiting VEGF release. Focal and grid laser treatments are recommended for different manifestations of diabetic maculopathy.
Surgical Interventions
Surgical intervention becomes essential in advanced stages of diabetic retinopathy. Pars plana vitrectomy (PPV) is employed to address complex scenarios such as tractional diabetic macular edema (DME) with non-proliferative diabetic retinopathy (NPDR). It involves the removal of the posterior hyaloid to relieve traction.
Additionally, PPV coupled with vitreous gel removal and endophotocoagulation is pivotal in addressing advanced proliferative diabetic retinopathy (PDR) with vitreous hemorrhage. For cases with extensive fibrovascular epiretinal membranes or tractional retinal detachment, PPV in combination with membrane removal, photocoagulation, and retinal reattachment measures offer effective outcomes.
Follow us in Facebook
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.