About White coat hypertension
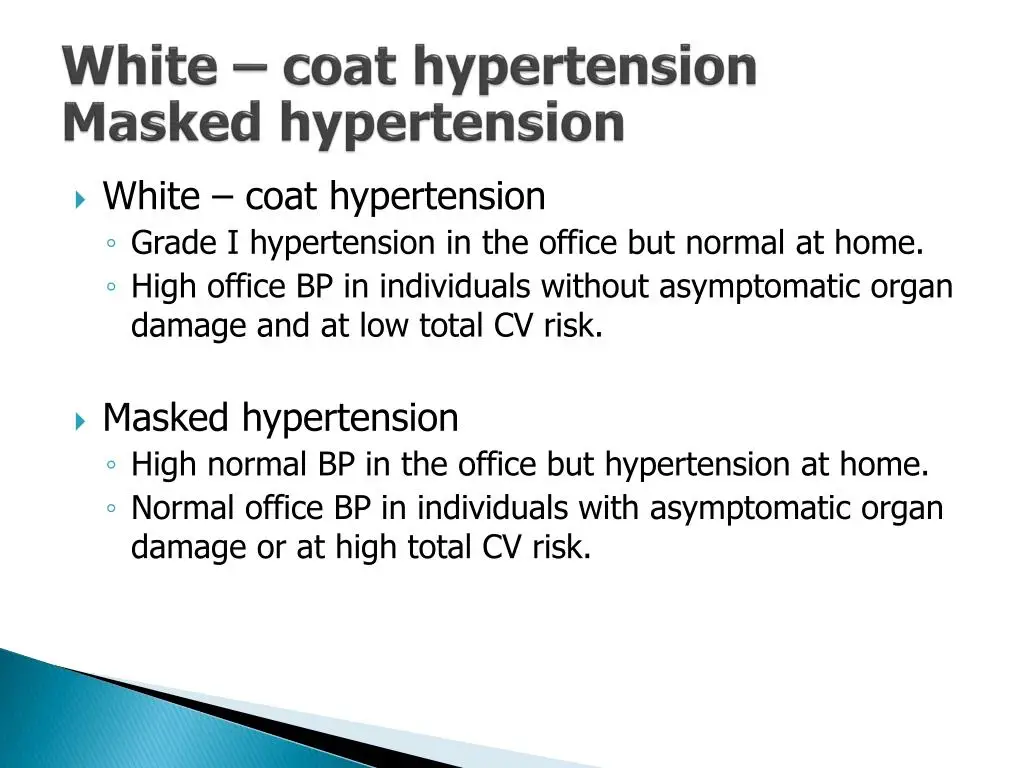
White coat hypertension (WCH), also known as isolated clinic hypertension, is a phenomenon where individuals exhibit elevated blood pressure readings in clinical settings, but have normal blood pressure levels outside of these settings.
How common is white coat hypertension(WCH)?

How common is white coat hypertension?
White coat hypertension affects 15% to 30% of people who have high blood pressure. People without high blood pressure can have it as well.
Prevalence rates have been reported to range from 15% to 40% in various population-based studies, depending on the diagnostic criteria and study populations. Factors such as age, gender, and comorbidities may influence the prevalence of white coat hypertension
Also read : New Genetic Mutation Behind Childhood Glaucoma Identified
Who gets white coat syndrome?
People who are more likely to have white coat syndrome include those who:
- Are older than 50.
- Were assigned female at birth.
- Were diagnosed recently with high blood pressure.
- Have obesity.
- Don’t use tobacco products.
Introduction to white coat hypertension(WCH)
Pic reference: my.clevelandclinic.org
Hypertension, a major risk factor for cardiovascular disease, affects a significant portion of the global population. However, the accuracy of blood pressure measurements in clinical settings has been a matter of debate. White coat hypertension, a well-documented phenomenon, poses challenges in accurately diagnosing and managing hypertension. This article aims to examine the prevalence and clinical implications of white coat hypertension, shedding light on its impact on patient care and long-term cardiovascular health.
Learn about more Eye diseases
Contributing Factors
Several factors contribute to the development of white coat hypertension. Psychological and emotional factors, including anxiety and stress, can significantly impact blood pressure measurements in clinical settings. Patient characteristics such as age, gender, and previous experiences with medical care may also influence the occurrence of white coat hypertension. Additionally, the white coat effect, wherein the presence of healthcare professionals induces a temporary rise in blood pressure, further contributes to the phenomenon.
Clinical Implications
White coat hypertension has important clinical implications. Misdiagnosis of hypertension can lead to unnecessary pharmacological treatment, exposing patients to potential adverse effects. Moreover, the psychological impact of being labeled as hypertensive can cause unnecessary anxiety and distress. Over time, these factors may negatively affect patient well-being and adherence to treatment plans.
Cardiovascular Risk and Management
While white coat hypertension is often considered a benign condition, recent evidence suggests that it may be associated with an increased risk of cardiovascular events. Long-term follow-up studies have shown that individuals with white coat hypertension may have a higher incidence of sustained hypertension and cardiovascular complications compared to normotensive individuals. Therefore, accurate identification and management of white coat hypertension are crucial to prevent potential long-term cardiovascular risks.
Diagnostic Approaches and Strategies
Various diagnostic approaches and strategies have been proposed to differentiate white coat hypertension from sustained hypertension. Ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) are considered reliable tools for obtaining out-of-office blood pressure measurements. These methods provide a more accurate assessment of blood pressure patterns, enabling healthcare professionals to make more informed treatment decisions.

Accurate diagnosis and management are essential to prevent unnecessary treatment and mitigate potential long-term cardiovascular risks. Incorporating ambulatory blood pressure monitoring and home blood pressure monitoring in clinical practice can help differentiate white coat hypertension from other diseases.
How to overcome white coat syndrome
Helping yourself feel more relaxed may bring your blood pressure closer to what it is at home.
These tips may help:
- Develop a good relationship with your healthcare provider so you can talk with them easily.
- If you don’t feel comfortable with your provider, find a different one.
- Bring a list of questions so you’re not anxious about forgetting to ask them.
- Allow extra time to get to your appointment and park so you don’t feel stressed.
- Don’t smoke, drink coffee or exercise for a half-hour before your appointment.
Ophthalmology and White Coat Hypertension
The intersection of White Coat Hypertension and ophthalmology bears particular relevance due to the frequent blood pressure measurements performed in clinical settings by ophthalmologists. The eyes, often regarded as windows to one’s overall health, can offer insights into cardiovascular well-being through conditions such as hypertensive retinopathy.
However, the presence of WCH necessitates caution and consideration when interpreting these findings. Ophthalmologists must acknowledge the potential influence of WCH on blood pressure readings, thereby enhancing diagnostic accuracy and ensuring appropriate patient management.
Follow us in Facebook for more updates
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.