Detecting Thyroid Eye Disease (TED)
What is Thyroid Eye Disease
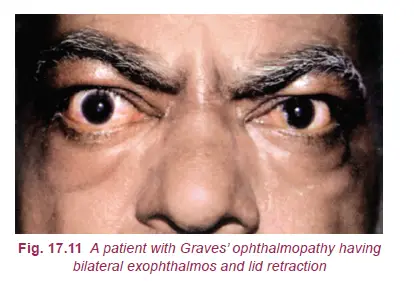
Sometimes, in thyroid patients, a condition develops in the eyes where the immune system starts to attack the tissues and other structures around the eyes. Due to thyroid eye disease, swelling occurs in the eyeball, making it appear as if the eyes are bulging out of their sockets. This swelling is caused by an autoimmune reaction, in which the body’s immune system targets the tissues surrounding the eyes.
In thyroid eye disease, immune cells attack the thyroid gland, which, in response, releases excessive thyroid hormones into the bloodstream. This leads to an enlarged thyroid gland and an increased metabolic rate. Symptoms of hypermetabolic state include rapid heartbeat, excessive sweating, high blood pressure, irritability, heat intolerance, weight loss, fatigue, hair loss, and changes in hair quality.
When the immune system attacks the tissues around the eyes, it often targets the muscles and connective tissues within and around the eye socket. This happens because these tissues contain proteins that resemble those found in the thyroid gland. The impact of this condition on the eyes can range from mild to severe, with the risk of vision loss occurring in only 10-20% of cases. Additionally, very few cases become severe or result in significant vision impairment.
Thyroid Eye Disease (TED) is sometimes known by other names:
- Thyroid-Associated Ophthalmopathy
- Thyroid Orbitopathy
- Graves Ophthalmopathy
- Graves’ Orbitopathy
Also read : Optometry blog
Thyroid Eye Disease (TED) Risk Factors
This condition is most commonly seen in hyperthyroid patients (77%), less frequently in euthyroid (20%) individuals, and rarely in hypothyroid (3%) patients. TED can occur before or after thyroid disease is diagnosed and, in most cases, symptoms develop within 18 months of each other. Although the seriousness and duration of this condition can vary significantly, TED is generally a self-limiting disease, lasting for about a year in non-smokers and up to three years in smokers.
TED typically occurs between the ages of 30 and 60. Women are five times more likely to develop it compared to men. However, when it does occur in men, the symptoms are often more advanced and severe, especially in older age. Smoking is the strongest risk factor, exacerbating the disease and making it more severe. This condition is less responsive to immunosuppressive therapy after exposure to radioactive iodine (RAI) treatment.
Previously, it was believed that the use of radioactive iodine (RAI) in the treatment of hyperthyroidism was linked to the development or worsening of TED. However, recent studies have suggested that RAI treatment can prevent the rapid progression of thyroid hormone stabilization following TED treatment.
Some research has suggested a genetic transmission of TED, but specific evidence confirming this link is still pending.
Identifying Symptoms
Symptoms may differ in severity from patient to patient. Early indicators include redness, dryness, or irritation in the eyes. You might feel as though you have something in your eyes, and you might become more sensitive to light. As the disorder progresses, symptoms often worsen. The eyelids may retract, causing more of the white of the eyes to show. Protrusion or “bulging” of the eyes is a common sign, which is a result of the inflammation and swelling in the eye sockets. You might experience blurred or double vision, and in severe cases, there can be sight loss.
Potential Complications
Over time, the swelling and inflammation can cause significant damage. Without treatment, Thyroid Eye Disease can lead to serious ocular complications. These can include corneal ulcers due to excessive dryness or poor eyelid coverage. The optic nerve may also become compressed, which can cause decreased vision or blindness.
Testing for Thyroid Eye Disease
The first step in testing is a complete eye examination. An eye care professional will check your vision, eye movements, and the appearance of your eyes. Checking for signs such as eyelid retraction and eye protrusion is crucial. An ophthalmologist may also use specific tests such as a color vision test, since changes in color vision can suggest optic nerve involvement.
Imaging tests play a significant role in the diagnosis of Thyroid Eye Disease. CT or MRI scans of the orbits are often used to confirm diagnosis and evaluate the extent of the disease.
Blood tests to measure thyroid hormone levels are essential. These can help link eye problems with an overactive thyroid. In certain cases, further diagnostic tests might be conducted, such as a thyroid scan to look for Graves’ Disease.
Remember, early detection and management can avoid serious eye problems and vision loss. It’s advised that anyone experiencing thyroid-related symptoms should seek medical consultation to rule out this condition. The treatment of Thyroid Eye Disease often involves a combination of approaches, aimed at reducing inflammation, managing symptoms, and if necessary, surgical intervention.
Although living with Thyroid Eye Disease can be distressing, many treatments exist to help manage the condition. With adequate medical care and self-care practices, people with this disease can maintain a good quality of life.
It’s essential to recognize the signs and symptoms of thyroid eye disease, but it’s equally crucial to understand that there are no official self-checks or at-home tests that can diagnose this condition accurately. Diagnosis requires the expertise of healthcare professionals and a series of clinical tests. However, having awareness of your symptoms and being prepared to communicate them with your healthcare provider is an essential first step in seeking proper diagnosis and treatment.
Recognizing Symptoms at Home
The initial step in identifying thyroid eye disease is to be aware of its common symptoms:
- Bulging or Protruding Eyes: Notice if your eyes appear more prominent than usual, which is a hallmark of the condition.
- Dry, Red, Sensitive, and Irritated Eyes: Be attentive to any persistent dryness, redness, or irritation in your eyes.
- Vision Changes: Keep track of any changes in your vision, such as double vision or blurriness.
- Pain or Pressure in Your Eyes: Be mindful of any discomfort, pain, or pressure in or around your eyes.
- Problems Moving Your Eyes: Pay attention to any difficulties in smoothly moving your eyes, especially if it leads to double vision.
- Watery Eyes: Note if your eyes become excessively watery, especially if it seems contradictory to other symptoms like dryness and irritation.
While these symptoms can be suggestive of thyroid eye disease, they can also be caused by various other eye conditions. Therefore, it’s crucial to consult with a healthcare professional for a proper evaluation and diagnosis.
Consulting a Healthcare Provider
When you experience any of these symptoms or notice other vision changes, it’s essential to reach out to a healthcare provider. The diagnostic process for thyroid eye disease typically involves the following steps:
1. Physical Examination:
Your primary care physician will conduct an initial physical examination, which may include checking for the following:
- The size and presence of nodules on your thyroid by palpation (touching the neck).
- Increased blood flow in the thyroid, known as a “thrill.”
- Listening to the sound of increased blood flow, called a “bruit,” with a stethoscope.
- Reflexes, heart rate, blood pressure, body temperature, skin, nails, hair, face, tremors or shaking, weight, and other relevant factors.
2. Eye Examination by an Ophthalmologist:
To assess the impact of thyroid eye disease on your eyes, you will need a comprehensive eye examination, including:
- Vision and color vision testing.
- Visual field testing.
- Eyelid measurements.
- Eye pressure readings.
- Evaluation of the optic nerves.
An ophthalmologist may also measure eye bulging using a device called an exophthalmometer, which quantifies how far forward your eyes have moved due to the condition.
3. Imaging Tests:
Imaging tests may be recommended to further evaluate your condition, such as:
- Radioactive iodine uptake test with X-rays to assess iodine collection by the thyroid.
- Ultrasound of the thyroid to detect enlargement or nodules.
- CT scan or MRI to check for thyroid enlargement and nodules, especially if Graves’ disease hasn’t been previously confirmed or to assess the condition of your eyes and eye muscles.
Thyroid Eye Disease symptoms
Symptoms of Thyroid Eye Disease
Thyroid Eye Disease (TED) is a condition that generally accompanies thyroid disorders, primarily Graves’ disease. Identifying its signs early can aid in reducing both its impact and the potential damage to the eyes, leading to more effective management of the condition.
Bulging Eyes
A common symptom of TED is bulging eyes or proptosis. This is caused by swollen muscles and fat tissues behind the eye, pushing it forward. Bulging can impact one or both eyes, and it may vary in severity. It’s crucial to consult an ophthalmologist if you notice any unusual protrusion in your eyes.
Red or Swollen Eyes
Redness or inflammation can occur either in the white area of the eyes or the eyelids. This symptom, sometimes accompanied by a sensation of grittiness in the eyes, can be an early warning sign of TED.
Excessive Tearing or Discomfort
Another noticeable symptom of TED is an increase in eye watering or tearing, often accompanied by discomfort. The eyes may also feel dry and irritated, leading to a burning sensation or the constant feeling of having something in your eye.
Light Sensitivity
People battling with TED may develop sensitivity to light. This hypersensitivity can range from a mild discomfort to severe pain when exposed to bright light.
Vision Blurring or Double Vision
Changes in vision, such as blurring or double vision (diplopia), are also indicative of TED. This may be due to the swelling of the muscles controlling eye movements, causing alignment problems.
Restricted Eye Movement
A less common but significant symptom of TED is restricted eye movement. As inflammation and swelling develop in the eye muscles, they become rigid, hindering the free movement of the eye. This can create pain or discomfort when trying to move the eyes in different directions.
Thyroid Eye Disease Treatment
For mild cases, you may be advised to lubricate your eyes with eye drops and use artificial tears several times a day. Avoid exposure to wind and bright light. If you experience serious symptoms, your doctor may prescribe corticosteroids such as prednisone to reduce swelling in your eyes. In some cases, orbital decompression surgery may be recommended. This procedure removes the bone between the eye socket and the air-filled sinus behind it to create more space for your eye. It can improve your vision, but there may still be a risk of double vision.
Double vision can occur when the eye disease affects the eye muscles severely, and eye muscle surgery may be used to correct vision and align the eyes properly. However, multiple surgeries may be required.
Now let’s discuss the best techniques for treating TED patients:
Non-surgical management of thyroid eye disease (TED) can be an essential part of the treatment plan to alleviate symptoms and manage the condition. Here are some key non-surgical approaches:
- Smoking Cessation: It is crucial to strongly encourage patients to quit smoking, as smoking can significantly impact the course of the disease. Smoking cessation can help prevent the exacerbation of TED symptoms.
- Elevated Head Position and Cold Compresses: Keeping the head elevated at night and applying cold compresses in the morning can help reduce periorbital edema (swelling around the eyes). This can provide relief from puffiness and discomfort.
- Artificial Tear Drops and Ointment: Lubricating artificial tear drops should be applied frequently during the day, and ointment can be used at bedtime. These help relieve symptoms such as dryness, foreign body sensation, and discomfort associated with dry ocular surfaces.
- Eyelid Taping: Taping the eyelids at night can help prevent complications of exposure, particularly in cases where the eyelids do not close properly.
- Guanethidine Eye Drops: Guanethidine 5% eye drops may be used to decrease lid retraction caused by the overaction of Muller’s muscle. These drops can help improve the appearance of the eyes.
- Prisms: Prisms may be prescribed to alleviate double vision (diplopia) that can occur during the active phase of TED. Prisms can help patients see more clearly and comfortably.
- Systemic Steroids: In cases of acutely inflamed orbit with rapidly progressive chemosis (swelling) and proptosis (bulging of the eyes) with or without optic neuropathy (damage to the optic nerve), systemic steroids may be indicated. These steroids can help reduce inflammation and alleviate symptoms.
- Radiotherapy: Radiotherapy, typically delivering 2000 rads over a 10-day period, may be considered to reduce orbital edema in cases where steroids are contraindicated or not effective. However, it’s important to note that radiotherapy may transiently worsen the disease before providing relief.
- Combined Therapy: Some patients may benefit from a combination of treatments, such as low-dose steroids, azathioprine (an immunosuppressive medication), and irradiation. This combined approach is reported to be more effective than using steroids or radiotherapy alone and can be considered in specific cases.
Some other treatment options on Detecting Thyroid Eye Disease
- Vitamin Supplements: Selenium supplements have been found effective in reducing the severity and progression of mild thyroid eye disease. It is recommended to start selenium supplementation as soon as possible during the disease, with an estimated benefit within the first 6 months. Vitamin D supplements have not been extensively researched in TED, but laboratory studies have shown an anti-inflammatory effect. Checking vitamin D levels and supplementing appropriately may be beneficial for patients. In addition, a good multivitamin and a healthy diet, especially low in processed foods and high in overall health, can be beneficial for gastrointestinal health, which can be compromised in TED.
- Topical Medications: Topical eye drops or ointments are often suggested for the treatment of ocular surface disease in TED. In the early and active stages, swelling on the eye’s surface is often a result of dry eyes, which can respond well to steroids like loteprednol or fluorometholone with low dosages. In the later stages after the disease, chronic exposure can cause dry eyes, which can be managed with lubrication. Artificial tears, gels, and nighttime ointments are often necessary, and surgery may eventually be required. Aggressive topical treatment can improve the quality of life for TED patients.
- Orbital Radiation: Radiation is helpful in cases where swelling persists continuously. Most of the time, it is prescribed in conjunction with steroids, as the combined effect of radiation and steroids is more than either alone. Common side effects include corneal dryness or the development of cataracts. Radiation can be especially helpful for patients who complain of squinting and double vision, though it does not shorten the course of active thyroid eye disease.
- Orbital Decompression: Orbital decompression surgery is the primary method of rehabilitation for TED patients. It can provide relief for nearly every complication caused by the disease, whether it’s site-threatening, optic nerve damage, or exposure keratopathy.
- Strabismus Surgery: Strabismus treatment surgery is quite common. It is usually performed to adjust the external muscles and improve double vision. However, strabismus surgery for TED can be more challenging compared to regular surgery. It is necessary to have this issue treated at a specialized eye hospital experienced in thyroid eye disease. The surgery typically takes about 30 to 60 minutes and can be performed under local anesthesia or topical anesthesia. It is performed on an outpatient basis. The improvement can vary depending on how many muscles were operated on in each patient.
- Eyelid Surgery: Eyelid surgery is often done as a last stage of rehabilitation for repairing the eyelid. It can be one of the most sensitive steps as the eyelid’s structure can be delicate and unpredictable. However, it is usually effective in making necessary improvements. This surgery is typically done under local anesthesia and may take 30 to 60 minutes. It is an outpatient procedure performed based on a patient’s individual needs.
- Cosmetic Surgery: TED mainly affects the tissues inside the orbit. This can result in significant changes in the appearance of the skin, brows, cheeks, neck, and other areas of the face. These changes can be addressed using a combination of laser treatments, fillers, Botox injections, or eyelid, brow, face, and neck surgeries.
Reference: AK khurana
Foolow us in Facebook
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.