Lacteocrumenasia (liquified after cataract)
Lacteocrumenasia is a term used to describe a specific complication that can arise after cataract surgery. The word itself combines “lacteo” (milky) and “crumena” (pouch or sac), indicating the presence of a milky fluid-filled sac in the eye following the surgical removal of the cataract. This condition is also commonly referred to as “liquified after cataract.”
Causes of Lacteocrumenasia:
The development of lacteocrumenasia is primarily attributed to the residual lens material left behind in the eye after cataract surgery. During the cataract removal procedure, the natural lens of the eye is replaced with an intraocular lens (IOL). However, in some cases, small fragments of lens material or lens epithelial cells may inadvertently remain within the eye.
Over time, these residual lens materials can undergo changes, leading to the formation of a milky fluid-filled sac or cyst. The fluid within this sac is often composed of liquefied lens proteins and inflammatory substances.
Clinical Presentation:
Lacteocrumenasia may not present with immediate symptoms after cataract surgery. Instead, it tends to manifest gradually, typically weeks to months after the initial procedure. Patients may report:
a. Decreased Vision: Patients may experience a decline in visual acuity, which can be attributed to the obstructive effect of the fluid-filled sac on light transmission to the retina.
b. Visual Disturbances: Some individuals may notice visual disturbances, such as glare or halos around lights, which can impact their visual quality.
c. Mild Discomfort: Some patients may report mild discomfort or a foreign body sensation in the affected eye.
Diagnosis:
Diagnosing lacteocrumenasia involves a comprehensive eye examination. Ophthalmologists will typically perform the following assessments:
a. Slit Lamp Examination: A slit lamp examination allows the ophthalmologist to visualize the presence of the milky fluid-filled sac within the eye. The sac is typically observed behind the iris and in front of the intraocular lens.
b. Fundus Examination: An examination of the retina helps rule out any other concurrent eye conditions and assess the impact of the lacteocrumenasia on retinal health.
c. Optical Coherence Tomography (OCT): OCT imaging may be used to obtain detailed cross-sectional images of the eye’s structures, aiding in the evaluation of the sac’s size and location.
Management:
The management of lacteocrumenasia involves addressing the underlying cause, which is the presence of residual lens material. Treatment options may include:
a. Neodymium-Doped Yttrium Aluminium Garnet (Nd:YAG) Laser Capsulotomy: Nd:YAG laser treatment can be used to create an opening in the posterior capsule of the lens. This allows the milky fluid within the sac to drain into the vitreous cavity, relieving the obstruction and improving visual symptoms. The procedure is non-invasive and typically safe.
b. Surgical Intervention: In cases where Nd:YAG laser capsulotomy is not feasible or effective, surgical removal of the fluid-filled sac may be considered. This procedure is more invasive but can provide relief from the visual disturbances caused by lacteocrumenasia.
Prognosis:
The prognosis for patients with lacteocrumenasia is generally favorable. Once the fluid-filled sac is drained or removed, visual symptoms usually improve. Nd:YAG laser capsulotomy is a relatively safe and effective procedure, and serious complications are rare.
Prevention:
Preventing lacteocrumenasia primarily involves thorough and careful cataract surgery. Ophthalmologists must ensure complete removal of the natural lens and any residual lens materials during the initial procedure.
Lacteocrumenasia (Case Report):
A patient is presented with milky fluid in the space between the posterior surface of an implanted intraocular lens (IOL) and the anterior surface of the distended posterior capsular bag
![]() Capsular bag distension syndrome (CBDS) is a rare complication of cataract surgery characterized by collection of turbid fluid between the posterior surface of the IOL and the posterior capsule.
Capsular bag distension syndrome (CBDS) is a rare complication of cataract surgery characterized by collection of turbid fluid between the posterior surface of the IOL and the posterior capsule.
![]() Lacteocrumenasia (liquified after cataract) is a type of CBDS occuring in the late postoperative period.
Lacteocrumenasia (liquified after cataract) is a type of CBDS occuring in the late postoperative period.
![]() Commonly CBDS presents with unexplained myopia, reduced vision, shallow anterior chamber and occasionally with high IOP.
Commonly CBDS presents with unexplained myopia, reduced vision, shallow anterior chamber and occasionally with high IOP.
![]() Presence of turbid fluid between the posterior capsule and the posterior surface of IOL and a fibrosed opacified rhexis margin adherent to the optic in this patient years after cataract surgery were features typical of late onset CBDS or lacteocrumenasia.
Presence of turbid fluid between the posterior capsule and the posterior surface of IOL and a fibrosed opacified rhexis margin adherent to the optic in this patient years after cataract surgery were features typical of late onset CBDS or lacteocrumenasia.
![]() Patient underwent neodymium yttrium aluminium garnet (ND-YAG) laser capsulotomy and the turbid fluid was released into the vitreous.
Patient underwent neodymium yttrium aluminium garnet (ND-YAG) laser capsulotomy and the turbid fluid was released into the vitreous.
![]() Photo:
Photo:
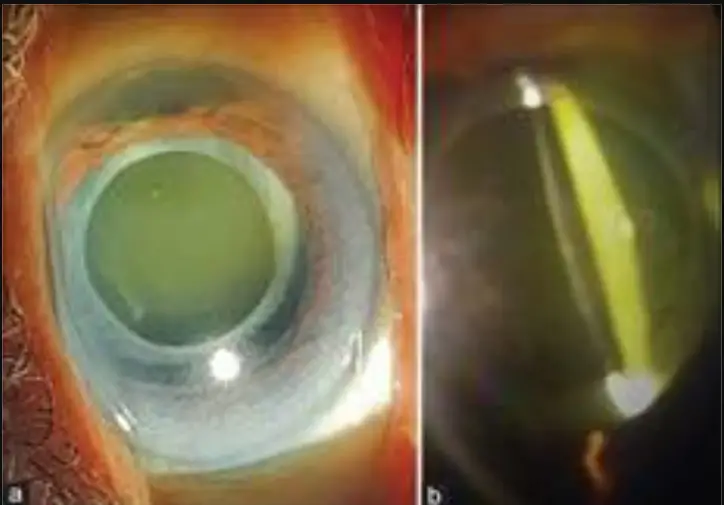
![]() Figure 1: (a and b) Shows the opacified anterior capsule rim adherent to the IOL optic and yellowish turbid fluid between the IOL and the posterior capsule.
Figure 1: (a and b) Shows the opacified anterior capsule rim adherent to the IOL optic and yellowish turbid fluid between the IOL and the posterior capsule.
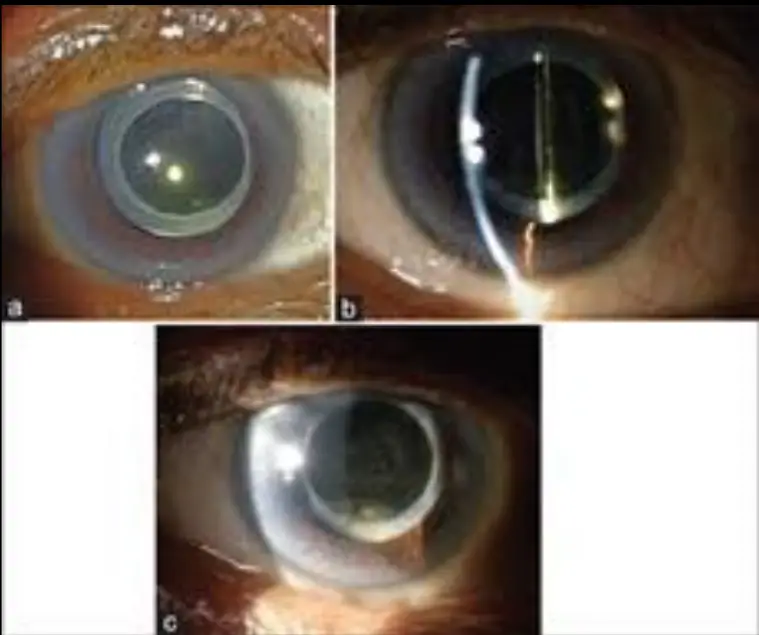
![]() Figure 2: (a-c) Shows the transparent IOL, disappearance of yellowish turbid fluid, posterior capsule opening and the whitish proliferation inferiorly behind the IOL.
Figure 2: (a-c) Shows the transparent IOL, disappearance of yellowish turbid fluid, posterior capsule opening and the whitish proliferation inferiorly behind the IOL.
More Case study :sciencedirect

You must be logged in to post a comment.