Superficial Punctate Keratitis (SPK):
superficial punctate keratitis: definition
Superficial punctate keratitis is an eye disorder caused by death of small groups of cells on the surface of the cornea (the clear layer in front of the iris and pupil).
![]() Superficial punctate keratoconjunctivitis is a very frequent finding as it can be caused by a wide variety of exogenous factors such as foreign bodies beneath the upper eyelid, contact lenses, smog, etc.
Superficial punctate keratoconjunctivitis is a very frequent finding as it can be caused by a wide variety of exogenous factors such as foreign bodies beneath the upper eyelid, contact lenses, smog, etc.
![]() It may also appear as a secondary symptom of many other forms of keratitis.
It may also appear as a secondary symptom of many other forms of keratitis.
![]() It can also occur in association with an endogenous disorder such as Thygeson’s disease.
It can also occur in association with an endogenous disorder such as Thygeson’s disease.
Superficial Punctate Keratitis symptoms:
![]() Depending on the cause and severity of the superficial corneal lesions, symptoms range from an early asymptomatic clinical course (such as in neuroparalytic keratitis in which the cornea loses its sensitivity) to an intense foreign body sensation in which the patient has a sensation of sand in the eye with typical signs of epiphora, severe pain, burning, and blepharospasm.
Depending on the cause and severity of the superficial corneal lesions, symptoms range from an early asymptomatic clinical course (such as in neuroparalytic keratitis in which the cornea loses its sensitivity) to an intense foreign body sensation in which the patient has a sensation of sand in the eye with typical signs of epiphora, severe pain, burning, and blepharospasm.
![]() Visual acuity is usually only minimally compromised.
Visual acuity is usually only minimally compromised.
Diagnostic considerations and differential diagnosis:
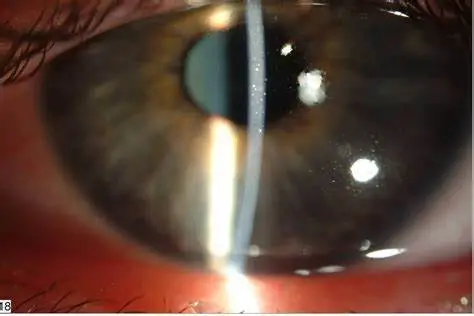
![]() Fluorescein dye is applied and the eye is examined under a slit lamp. This visualizes fine epithelial defects.
Fluorescein dye is applied and the eye is examined under a slit lamp. This visualizes fine epithelial defects.
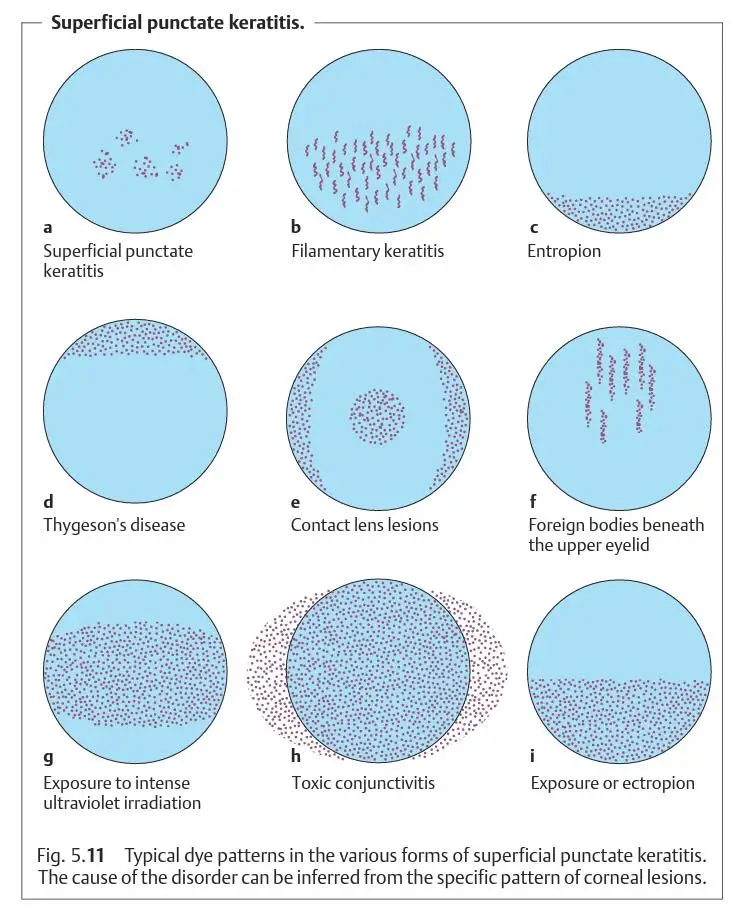
![]() The specific dye patterns that emerge give the ophthalmologist information about the etiology of the punctate keratitis.
The specific dye patterns that emerge give the ophthalmologist information about the etiology of the punctate keratitis.
What are the causes of keratitis?
The cause of superficial punctate keratitis may be any of the following:
- A viral infection
- A bacterial infection (including trachoma)
- Dry eyes
- Strong chemicals splashed in the eye
- Exposure to ultraviolet light (sunlight, sunlamps, or welding arcs)
- Prolonged use of contact lenses
- An allergy to eye drops
- Blepharitis (eyelid inflammation)
- Bell palsy
- A side effect of certain drugs taken by mouth (orally) or by vein (intravenously)
Treatment and prognosis of Superficial Punctate Keratitis:
![]() Depending on the cause, the superficial corneal changes will respond rapidly or less so to treatment with artificial tears, whereby every effort should be made to eliminate the causative agents.
Depending on the cause, the superficial corneal changes will respond rapidly or less so to treatment with artificial tears, whereby every effort should be made to eliminate the causative agents.
![]() Depending on the severity of findings, artificial tears of varying viscosity (ranging from eyedrops to high-viscosity gels) are prescribed and applied with varying frequency.
Depending on the severity of findings, artificial tears of varying viscosity (ranging from eyedrops to high-viscosity gels) are prescribed and applied with varying frequency.
![]() In exposure keratitis, a high-viscosity gel or ointment is used because of its long retention time; superficial punctate keratitis is treated with eyedrops.
In exposure keratitis, a high-viscosity gel or ointment is used because of its long retention time; superficial punctate keratitis is treated with eyedrops.
Thygeson’s Superficial Punctate Keratitis
Thygeson’s Superficial Punctate Keratitis tspk is a chronic eye disorder first described by Phillips Thygeson in 1950. This condition is characterized by small, raised oval corneal opacities that are whitish-gray in color and can be found across the entire front surface of both eyes. These lesions often concentrate in the central part of the cornea and are associated with mild or absent inflammation in the conjunctiva. TSPK typically occurs in the second to third decade of life, with a higher incidence in females, but its prevalence is likely underestimated due to limited publications.
The exact cause of TSPK is still unclear, with both viral and immunological factors implicated. Some studies have suggested viruses like adenovirus, herpes simplex virus, and varicella-zoster virus as potential triggers, but the evidence is inconclusive. An immune-based explanation has also been proposed, as patients with TSPK have been found to have a specific genetic marker (HLA-DR3) associated with immune response genes and autoimmune disorders.
Symptoms of TSPK include photophobia, tearing, burning, foreign body sensation, and irritation, often accompanied by pain and blurred vision during exacerbations. The disease can be bilateral but may vary in severity between the eyes. Episodes can last from 1 to 2 months, with remission periods lasting up to 6 weeks. In most cases, the condition tends not to recur after about 4 years, although there are reports of longer-lasting cases, with one lasting 41 years.
TSPK presents as gray-white, oval-shaped lesions within the corneal epithelium, with minimal inflammation and edema in the underlying stroma. These lesions may or may not stain with certain dyes like fluorescein, rose bengal, or lissamine green. They tend to disappear within 4 to 6 weeks, and corneal sensitivity is usually preserved or slightly reduced. While the conjunctiva usually remains calm, some patients may experience redness and filament formation in a few cases. In advanced stages, subepithelial fibrosis or anterior stromal scarring may develop.
Treatment options for Thygeson’s Superficial Punctate Keratitis (TSPK) have been explored, but none have proven entirely successful. Antibiotics have shown little effectiveness, and antivirals like trifluridine offer mixed results. Idoxuridine is contraindicated due to causing persistent scarring.
Topical lubricants can help relieve symptoms partially, but the mainstay of treatment is topical corticosteroids. They effectively control both clinical signs and symptoms, although there are concerns they may prolong the disease. Corticosteroids must be tapered gradually over a long period to achieve a regular, infrequent dose.
Topical cyclosporine (CsA) is suggested as a first-line treatment due to its therapeutic success and safety compared to corticosteroids, although it hasn’t been compared directly in clinical trials. Stinging at instillation can be an issue with CsA. Topical tacrolimus and ointment are other steroid-sparing options.
For severe TSPK, extended-wear soft contact lenses may be an alternative, improving symptoms by covering the corneal lesions. However, they carry a risk of complications like microbial keratitis.
Excimer laser phototherapeutic keratectomy (PTK) has been attempted in some cases, but it offers only partial improvement with a high rate of lesion recurrence, making it less suitable for managing the disease.
Credit: Lang-Ophthalmology: A Short Textbook.
Are you an Eye Professional? Register yourself in our Eye professional directory for Free.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.