Macular degeneration are major causes of blindness. In developed countries, blindness today is rarely caused by infection or malnutrition but mainly by degenerative, metabolic and vascular conditions affecting the macula.
Macular degeneration occurs when the macula, which is the central part of the retina responsible for sharp, detailed vision, deteriorates over time. This deterioration can cause blurred or distorted vision, difficulty reading, and even blindness in severe cases.
While there is no cure for macular degeneration, early detection and treatment can help slow its progression and preserve vision.
Anatomy of the Eye and the Macula

The eye is a complex organ that allows us to see the world around us. It works by capturing light and converting it into electrical signals that are sent to the brain. The macula is a small, specialized area located in the center of the retina, which is the part of the eye responsible for sensing light.
The macula is made up of millions of light-sensitive cells called photoreceptors. These cells are divided into two types: rods and cones. Rods are responsible for detecting light and dark, while cones are responsible for detecting color. The macula contains mostly cones, which makes it particularly important for detailed vision and color perception.
The macula is also surrounded by a network of blood vessels that supply it with oxygen and nutrients. This network is called the choroid, and it plays an important role in maintaining the health of the macula.
Common chronic macular lesions
Common chronic macular lesions which cause gradual loss of central vision include degenerative high myopia, juvenile macular dystrophy and age-related macular degeneration. The common acute macular conditions are central serous retinopathy, macular
haemorrhages, and disciform macular degeneration. Diffuse retinal conditions which affect the macula include retinal vein occlusion and diabetic retinopathy.
Types of Macular Degeneration
Macular degeneration is a condition that affects the macula, which is the part of the eye responsible for central vision.
There are two main types of macular degeneration: dry and wet.
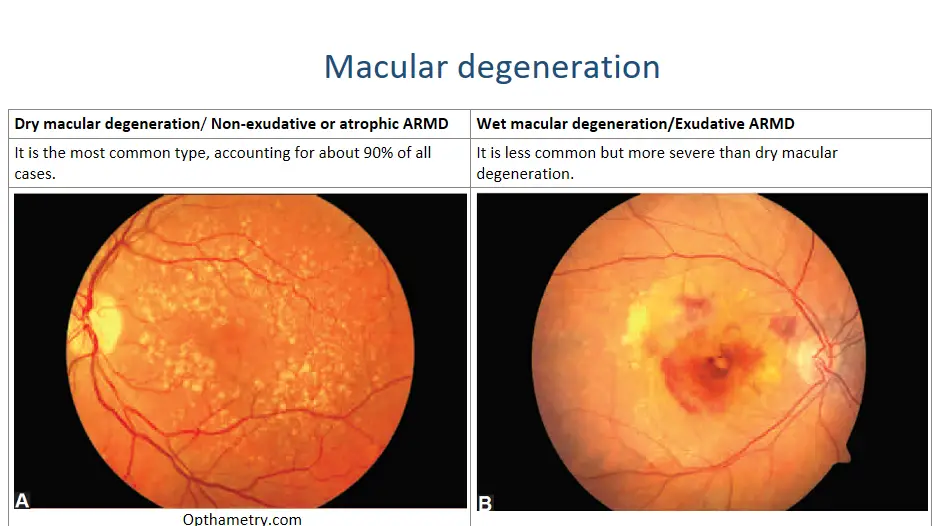
Dry macular degeneration/ Non-exudative or atrophic ARMD is the most common type, accounting for about 90% of all cases. It occurs when the cells in the macula break down and waste products accumulate, causing the macula to thin and dry out. This can lead to blurred or distorted vision, as well as blind spots in the center of the visual field.

Dry macular degeneration/ Non-exudative or atrophic ARMD
Wet macular degeneration/Exudative ARMD is less common but more severe than dry macular degeneration. It occurs when abnormal blood vessels grow under the retina and leak fluid or blood, causing damage to the macula. This can lead to rapid loss of central vision and may require urgent treatment to prevent further damage.

Wet macular degeneration/Exudative ARMD
Both types of macular degeneration can occur in one or both eyes, and they typically affect people over the age of 50. While there is no cure for macular degeneration, early detection and treatment can help slow its progression and preserve vision.
Risk Factors for Macular Degeneration
Macular degeneration is a complex eye condition that can affect anyone, but certain risk factors increase the likelihood of developing it. Age is the most significant risk factor for macular degeneration, with the majority of cases occurring in people over the age of 60. Other risk factors include smoking, obesity, high blood pressure, and a family history of the disease.
People with lighter skin and eye color are also at a higher risk of developing macular degeneration. Additionally, prolonged exposure to sunlight and a diet low in antioxidants and omega-3 fatty acids may increase the risk of developing this condition. It’s important to be aware of these risk factors and take steps to reduce them where possible to help prevent or delay the onset of macular degeneration.
Age-related maculopathy (senile macular degeneration)
Age-related maculopathy (senile macular degeneration) is a bilateral degeneration of the macula. It causes loss of central vision. It accounts for over 20% of blindness in Caucasians (less than 6/60 visual acuity) but is less prevalent in other races. The patient usually complains of gradual increasing disturbance of central vision. One letter or word may appear at a different level from its neighbour or there may be missing letters or words.
The ophthalmoscopic picture varies. The macula usually has fine pigmentary clumps and patches of atrophy. White round spots called drusen (colloid bodies) are frequently seen. They are waste deposits located just beneath the retinal pigment epithelium. Drusen by themselves are usually harmless, especially if they are few in number and are sharply-demarcated. Large or confluent drusen are frequently associated with macular degeneration. Sometimes, vision may be suddenly lost because of an acute complication of age-related maculopathy.

drusen in macular degeneration (AK Khurana)
A localised, raisedexudative lesion due to subretinal bleeding from new vessel proliferation from the choroid (subretinal neovascularisation) may develop at the macula. If untreated, this may lead to scarring and loss of vision.
Urgent fundal fluorescein angiographic tests should be carried out, as subretinal neovascularisation at an early stage may be effectively treated with laser photocoagulation.
It is important to emphasize to patients with macular degeneration that they will not go totally blind from the condition as peripheral vision will not be affected. Some patients benefit from the use of strong glasses and a variety of visual aids for distant and near vision. These include magnifying lenses and special telescopic spectacles
The Role of Genetics in Macular Degeneration
Macular degeneration is a complex disease that can be influenced by various factors, including genetics. While age-related macular degeneration (AMD) is the most common type of the disease, there are also genetic forms of macular degeneration that can affect individuals at a younger age.
Studies have shown that certain genes can increase an individual’s risk of developing AMD. The complement factor H (CFH) gene, for example, has been identified as a major genetic risk factor for AMD. Other genes, such as ARMS2/HTRA1 and C3, have also been linked to an increased risk of developing the disease.
It’s important to note that having these genetic risk factors does not necessarily mean an individual will develop macular degeneration. Environmental factors, lifestyle choices, and other health conditions can also play a role in the development of the disease.
Genetic testing is available for some forms of macular degeneration, but it’s important to discuss the potential benefits and limitations of testing with a healthcare provider or genetic counselor. Understanding one’s genetic risk for macular degeneration can help individuals make informed decisions about their eye health and potentially take steps to reduce their risk of developing the disease.
Prevention and Treatment of Macular Degeneration
Prevention and treatment of macular degeneration are crucial to maintaining good eye health. While there is no cure for the disease, there are steps you can take to reduce your risk of developing it or slow its progression if you have already been diagnosed.
One of the most important things you can do to prevent macular degeneration is to maintain a healthy lifestyle. This includes eating a balanced diet rich in fruits and vegetables, exercising regularly, not smoking, and protecting your eyes from harmful UV rays by wearing sunglasses.
Treatment of non-exudative ARMD: Currently, there is no effective treatment that stop progression of dry AMD. Measures to be tried include:
- Dietary supplements and antioxidants. The agerelated eye disease study (AREDS) has suggested that use of certain specific antioxidants, vitamins and minerals [vitamin C (500 mg) and vitamin E (400 IU), beta carotene (15 mg), zinc oxide (80 mg) and cupric oxide (2 mg)] could possibly prevent or delay the progression of ARMD.
- Smoking cessation may slow down the progress.
- Amsler grid used regularly allows the patients to detect new or progressive metamorphopsia prompting them to seek ophthalmic advice.
- Refraction with increased near add may be helpful in early cases.
- Low vision aid may be needed in advanced cases of geographical atrophy. low vision aids that can help individuals with macular degeneration continue to perform daily tasks such as reading and driving. These include magnifying glasses, telescopes, and computer programs that enlarge text and images.
It’s important to remember that early detection and treatment are key to managing macular degeneration. Regular eye exams with an ophthalmologist or optometrist can help detect the disease in its early stages and allow for prompt treatment. By taking steps to prevent and treat macular degeneration, you can help protect your vision and maintain your quality of life.
Understanding the Progression: The Three Stages of Macular Degeneration and How to Manage Them
There are three stages of macular degeneration: early, intermediate, and advanced. Each stage has its own set of symptoms and treatment options. Understanding the progression of macular degeneration is crucial for managing the disease effectively. In this article, we will discuss each stage of macular degeneration in detail and explore the various treatment options available. We will also provide tips on how to prevent and manage macular degeneration to maintain good eye health.
- Early Stage Macular Degeneration
Early stage macular degeneration is the beginning phase of the disease. It’s often difficult to detect as there may be no noticeable symptoms. However, it’s important to get regular eye exams as early detection can lead to better management and treatment options. In this stage, small yellow deposits called drusen may start to form in the macula, which is the central part of the retina responsible for sharp, clear vision.
These deposits can cause slight blurring or distortion in your vision, especially when reading or looking at fine details. If you notice any changes in your vision, such as difficulty seeing in low light or needing brighter light to read, it’s important to schedule an appointment with your eye doctor. They can perform a comprehensive eye exam and determine if you have early stage macular degeneration.
2. Intermediate Stage Macular Degeneration
During the intermediate stage of macular degeneration, the symptoms become more noticeable and pronounced. Patients may experience blurred or distorted vision, difficulty reading, and a need for brighter lighting. Straight lines may appear wavy or crooked, and there may be blind spots in the central vision.
At this stage, it is important to continue regular eye exams and monitoring by an ophthalmologist. The doctor may recommend using low vision aids such as magnifying glasses or special lenses to help with reading and other daily activities.
It is also crucial to maintain a healthy lifestyle and diet, including eating foods rich in vitamins A, C, and E, zinc, and omega-3 fatty acids. Quitting smoking and protecting the eyes from harmful UV rays can also slow down the progression of macular degeneration.
In some cases, the doctor may recommend treatments such as injections of anti-VEGF drugs or photodynamic therapy to slow down the growth of abnormal blood vessels in the eye. However, these treatments are not always effective and may have side effects.
Overall, managing intermediate stage macular degeneration requires a combination of medical treatment and lifestyle changes. With proper care and attention, patients can maintain their quality of life and preserve their vision for as long as possible.
3. Advanced Stage Macular Degeneration
At the advanced stage of macular degeneration, vision loss becomes severe and can significantly impact daily activities. In this stage, central vision is severely affected, making it difficult to recognize faces, read, or drive. Some individuals may experience a blind spot in the center of their vision, while others may have distorted or wavy vision.
Unfortunately, there is no cure for advanced stage macular degeneration. However, there are treatment options that can help slow down the progression of the disease and manage its symptoms. One such option is low vision aids, which can include magnifying glasses, telescopes, and electronic devices that enlarge images. These aids can help individuals with advanced stage macular degeneration perform daily tasks more easily.
Another treatment option is photodynamic therapy, which involves injecting a light-sensitive drug into the bloodstream and then using a laser to activate the drug in the eye. This treatment can help slow down the growth of abnormal blood vessels in the eye, which can cause further damage to the macula.
In some cases, surgery may be an option for advanced stage macular degeneration. One such surgery is a retinal transplant, which involves replacing the damaged retina with a healthy one from a donor. However, this procedure is still experimental and not widely available.
Overall, managing advanced stage macular degeneration requires a team approach involving an ophthalmologist, low vision specialist, and other healthcare professionals. It’s important to work closely with your healthcare team to develop a personalized treatment plan that addresses your specific needs and goals.
Summary: The Options for Treating Macular Degeneration
There are several current treatment options available for macular degeneration. These treatments aim to slow down the progression of the disease and prevent further vision loss. The most common treatments include:
- Anti-VEGF Injections: This treatment involves injecting a medication into the eye that blocks the growth of abnormal blood vessels in the retina. This helps to reduce swelling and bleeding in the eye, which can improve vision. Anti-VEGFs are injected intravitreally. These include: Bevacizumab (Avastin), dose: 1.25 mg, or Ranibizumab (Lucentis), dose: 0.5 mg/0.05 ml, or Pegaptanib (Macugen), dose: 0.3 mg in 90 ml
- Laser Therapy: This treatment uses a high-energy laser to destroy abnormal blood vessels in the retina. This can help to slow down the progression of the disease and prevent further vision loss.
- Photodynamic Therapy/ PDT: This treatment involves injecting a medication into the bloodstream that is activated by a laser. PDT is the treatment of choice after anti-VEGF injections for subfoveal and juxtafoveal classic CNVM. The laser is then used to destroy abnormal blood vessels in the retina.
- Transpupillary thermotherapy (TTT) with a diode laser (810 nm) may be considered for subfoveal occult CNVM. PDT is definitely better than TTT but is very expensive.
- Double frequency and YAG 532 nm photocoagulation may be used for extrafoveal choroidal neovascular membrane (CNVM).
- Surgical treatment. Submacular surgery to remove CNVM and macular translocation surgery are being evaluated.
- Vitamins and Supplements: Certain vitamins and supplements, such as vitamin C, vitamin E, zinc, and copper, may help to slow down the progression of macular degeneration.
Pros and cons of various methods
anti-VEGF injections : These injections work by blocking the growth of abnormal blood vessels in the eye, which can slow down or even stop the progression of macular degeneration. One of the main benefits of this treatment is that it is minimally invasive and can be done in an outpatient setting. However, some patients may experience side effects such as eye pain, redness, or inflammation.
photodynamic therapy (PDT). This involves injecting a light-sensitive drug into the bloodstream, which is then activated by a laser to destroy abnormal blood vessels in the eye. PDT can be effective for certain types of macular degeneration, but it is not suitable for everyone. It can also cause temporary vision loss and sensitivity to light.
Laser therapy is another option for treating macular degeneration. This involves using a laser to destroy abnormal blood vessels in the eye. While this treatment can be effective, it can also cause scarring and damage to healthy tissue.
In some cases, surgery may be necessary to treat macular degeneration. One surgical option is a vitrectomy, which involves removing the gel-like substance in the eye and replacing it with a saline solution. This can help improve vision in some patients, but it is a more invasive procedure that carries risks such as infection and bleeding.
It is important to note that these treatments may not work for everyone and may have potential side effects. It is important to discuss the risks and benefits of each treatment option with your doctor before making a decision.
what foods should be avoided with macular degeneration
Nutrition plays a crucial role in maintaining eye health, especially when it comes to macular degeneration.
- The macula requires specific nutrients to function correctly, such as lutein and zeaxanthin. These are found in leafy green vegetables like spinach and kale. These nutrients act as antioxidants, protecting the macula from harmful free radicals that can cause damage over time.
- vitamins C and E, zinc, and omega-3 fatty acids also helps to keep the eyes healthy. These nutrients can be found in various foods such as citrus fruits, nuts, seed.
- include fish in your diet, particularly those that are rich in omega-3 fatty acids such as salmon, tuna, and mackerel. These fatty acids have been shown to reduce inflammation in the body, including the eyes, and may also help prevent age-related macular degeneration.
A diet rich in these nutrients can help reduce the risk of developing macular degeneration and slow down its progression in those who already have the condition. But sadly it cannot reverse any damage that has already occurred. Therefore, it’s crucial to start implementing healthy eating habits as early as possible to prevent any future damage to the eyes.
Foods to Avoid with Macular Degeneration
Just like certain foods can help slow down its progression similarly some foods can worsen the condition and should be avoided.
Food you should avoid are:
- Processed and packaged foods. These foods are often high in saturated and trans fats, which can increase inflammation in the body and contribute to the development of age-related diseases such as macular degeneration. Examples of these foods include chips, cookies, cakes, and other snacks that come in bags or boxes.
- red meat. Red meat is high in saturated fat and cholesterol, which can clog arteries and reduce blood flow to the eyes. Instead, opt for lean protein sources such as fish, poultry, and plant-based proteins like beans and lentils.
- limit your intake of refined carbohydrates such as white bread, pasta, and rice. These foods have a high glycemic index, which means they can cause a rapid spike in blood sugar levels. High blood sugar levels can damage blood vessels in the eyes and contribute to the development of macular degeneration.
By avoiding or limiting these foods, you can help protect your eyesight and slow down the progression of macular degeneration.
Follow us via Facebook to read more Interesting eye articles

You must be logged in to post a comment.