Understanding CMV Retinitis: Clinical Examination and Lesion Characteristics
CMV Retinitis eye problem and AIDS
Cytomegalovirus (CMV) retinitis is a sight-threatening infection commonly seen in immunocompromised individuals, particularly those with advanced HIV/AIDS. Early detection and management are crucial to prevent vision loss and potential complications. A comprehensive ocular examination is essential for diagnosing and managing CMV retinitis effectively. Here, we explore the clinical examination process and the characteristic features of retinal lesions associated with CMV retinitis.
Ocular Examination for Suspected CMV Retinitis:
Patients suspected of CMV retinitis should undergo a thorough ocular examination, encompassing various aspects of visual function and ocular health:
- Visual Acuity Assessment: Establishing baseline visual acuity is essential for monitoring disease progression and treatment response.
- Visual Field Testing: Detection of visual field defects helps in assessing optic nerve damage, retinal detachment, or central nervous system involvement.
- Ocular Motility and Cranial Nerve Examination: Evaluation of ocular motility aids in detecting any cranial nerve abnormalities, which may indicate CNS diseases associated with AIDS.
- Pupil Examination: Checking for relative afferent pupillary defects can provide insights into optic nerve involvement.
- External Examination: External examination of the lids and adnexa may reveal signs of other AIDS-associated conditions, such as Kaposi sarcoma or lymphoma.
- Anterior Segment Examination: Assessing the anterior chamber for signs of uveitis, including elevation or depression of intraocular pressure, is crucial. CMV retinitis may present with nonspecific uveitis.
- Slit Lamp Examination: Fine, stellate keratitic precipitates characteristic of CMV may be observed on the corneal endothelium. Presence of uveitis may require treatment.
- Vitreous Evaluation: Assessment of vitreous inflammation aids in monitoring treatment response and detecting immune recovery uveitis (IRU) with severe anterior and posterior uveitis post-HAART initiation.
- Dilated Fundus Examination: Indirect ophthalmoscopy allows for the evaluation of retinal lesions’ location, extent, and associated complications such as retinal breaks or detachment.
Characteristics of CMV Retinitis Lesions:
Retinal lesions in CMV retinitis exhibit several distinctive features, aiding in diagnosis and monitoring:
- Perivascular Distribution: Initial lesions are typically perivascular, reflecting hematogenous spread of the virus.
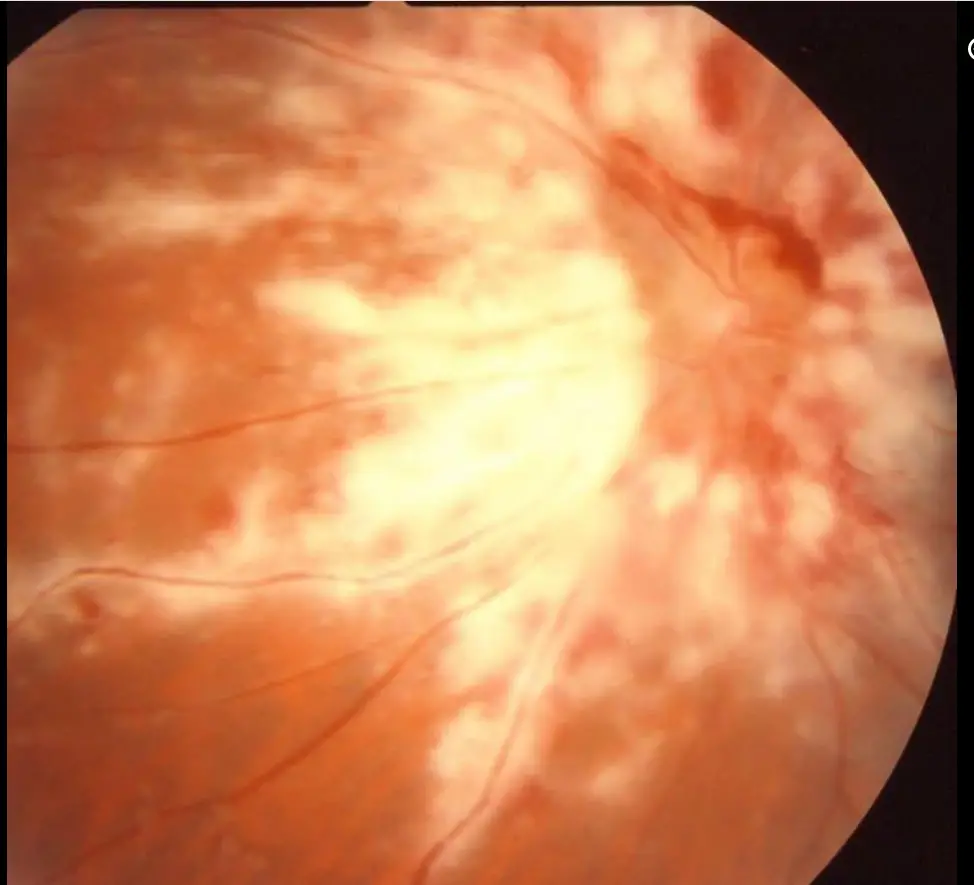
- Appearance: Posterior lesions present as large areas of thick white infiltrate along retinal vessels, often accompanied by hemorrhage, resembling a “pizza pie” or “cheese pizza.”
- Peripheral Lesions: These have a more granular appearance with satellite lesions and minimal hemorrhage. Necrotic retina with mottled pigmentation from hyperplasia of the retinal pigment epithelium (RPE) is seen behind the advancing border.
- Progression: Lesions usually begin peripherally and spread posteriorly, following the nerve fiber layer.
- Minimal Vitreitis: Even severe retinitis is typically accompanied by minimal vitreitis in immunocompromised patients.
- Vascular Sheathing: Extensive vascular sheathing, termed frosted branch angiitis, may occur but is uncommon.
- Vascular Occlusion: Retinal vascular occlusion or nonperfusion can be observed on fluorescein angiography or direct examination.
- Peripheral Holes and Tears: These frequently occur within areas of necrosis.
In summary, Retinal lesions in CMV retinitis exhibit distinct characteristics:
- Initial presentation typically reveals 1 or 2 focal points of disease, with multifocal disease being uncommon.
- Early lesions commonly manifest in a perivascular distribution, suggestive of hematogenous viral dissemination.
- Posterior lesions present as large, thick white infiltrates along retinal vessels, often accompanied by hemorrhage, resembling a “pizza pie” or “cheese pizza” appearance.
- Peripheral lesions display a granular appearance with satellite lesions and less hemorrhage. Necrotic retina with mottled pigmentation from RPE hyperplasia is observed behind the advancing border.
- Lesions typically begin peripherally and spread posteriorly in a contiguous fashion, although multiple unconnected lesions are also frequent. Involvement of the posterior pole with minimal peripheral disease occurs in 5-10% of cases.
- Retinitis follows the nerve fiber layer, leading to wide areas of necrosis, scarring, and atrophy.
- Severe retinitis is usually accompanied by minimal vitreitis in immunocompromised patients. However, HAART initiation may lead to immune reconstitution uveitis (IRU) with severe anterior and posterior uveitis.
- Frosted branch angiitis, characterized by extensive vascular sheathing, is an uncommon appearance.
- Retinal vascular occlusion or nonperfusion may be observed on fluorescein angiography or direct examination.
- Peripheral holes and tears are common within areas of necrosis.
In summary, a comprehensive ocular examination, coupled with an understanding of the characteristic features of CMV retinitis lesions, is vital for early detection, accurate diagnosis, and effective management of this potentially blinding condition in immuno compromised individuals. Regular monitoring and prompt intervention are essential to preserve visual function and improve patient outcomes.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.