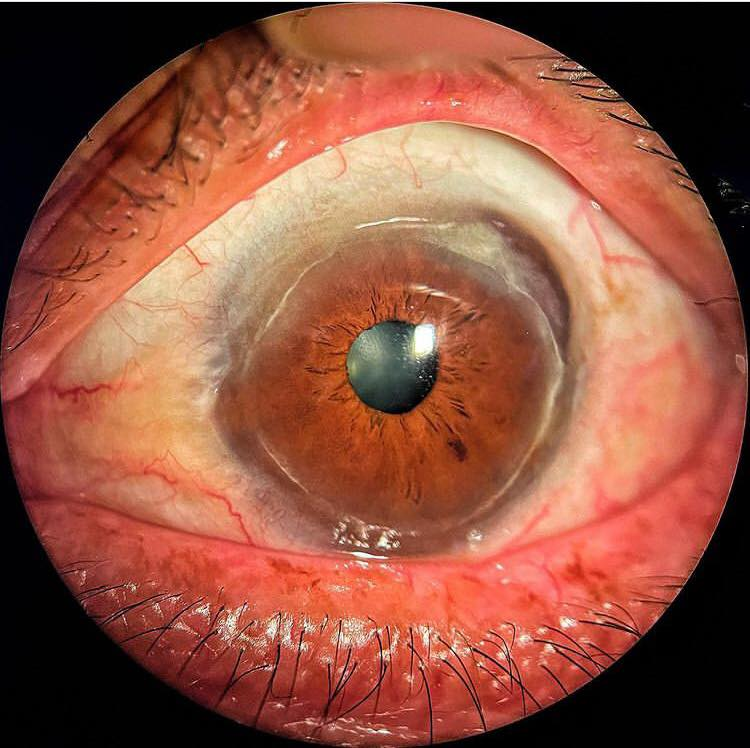
Terrien’s Marginal Corneal Degeneration:
Terrien’s marginal degeneration is an uncommon but distinct variety of peripheral corneal thinning of the cornea. It causes a slowly progressive non-inflammatory, unilateral or asymmetrically bilateral peripheral corneal thinning and is associated with corneal neovascularization, opacification and lipid deposition. Marginal Corneal Degeneration may lead to a high degree of against-the-rule or oblique astigmatism.
Corneal thinning can be localized or involve extensive proportions of the peripheral cornea. Degeneration typically begins superiorly with mild, punctuate subepithelial and/or anterior stromal opacities and leaves a clear area between the opacities and the limbus. Opacification is followed by the development of a peripheral, superficial, fine vascular pannus, which progresses over the years to include subepithelial opacity at the advancing edge, without the overlying edge characteristic of Mooren’s ulcer. The thinning spreads circumferentially, rarely involves the inferior limbus, and leaves the epithelium intact.
The central wall is steep, and the peripheral wall slopes gradually. A yellow line of lipid deposits appears at the leading edge of the pannus (central edge of the furrow). Vessels transverse the furrow and pass beyond it. Spontaneous perforation is rare, although perforation can occur easily with minor trauma. Spontaneous ruptures in Descemet’s membrane can result in interlamellar fluid or even a corneal cyst.

Physical Examination of Terrien’s Marginal Corneal Degeneration:
Physical examination reveals a leading edge of lipid, steep central edge, sloping peripheral edge, intact epithelium and superficial vascularization. Patients have a high against-the-rule or oblique astigmatism from the progressive flattening of the vertical meridian.
Terrien’s marginal degeneration symptoms
Typically presents as painless progressive blurred vision.
Clinical Diagnosis of Terrien’s Marginal Corneal Degeneration:
Terrien’s marginal degeneration may be differentiated from other peripheral corneal thinning disorders by the lack of inflammation, presence of superficial vascularization, advancing linear deposition of lipid, lack of epithelial defect and slow progressive course. It can present with recurrent painful episodes of inflammation. Collagen vascular diseases should be excluded. No known systemic associations
Notes on Terrien’s Marginal Corneal Degeneration
![]() Terrien’s marginal degeneration is a peripheral inflammatory condition often included in the degenerative category.
Terrien’s marginal degeneration is a peripheral inflammatory condition often included in the degenerative category.
terrien’s marginal degeneration causes:
It is a rare disorder of unnown etiology.
![]() The condition can be seen at any age but is most common in those between 20 and 40 years of age. Men are affected more than women in a 3:1 ratio.
The condition can be seen at any age but is most common in those between 20 and 40 years of age. Men are affected more than women in a 3:1 ratio.
![]() Typically, the disease is bilateral and symmetric, but may be asymmetric, with disease occurring in the second eye decades after the first.
Typically, the disease is bilateral and symmetric, but may be asymmetric, with disease occurring in the second eye decades after the first.
![]() The lesion usually begins superonasally with fine punctate opacities in the anterior stroma with a lucent area to the limbus. Fine superficial vasculariation from the limbal arcades leading to the lesion differentiates it from arcus.
The lesion usually begins superonasally with fine punctate opacities in the anterior stroma with a lucent area to the limbus. Fine superficial vasculariation from the limbal arcades leading to the lesion differentiates it from arcus.
![]() A gutter similar to marginal furrow degeneration then forms between the opacity and limbus.
A gutter similar to marginal furrow degeneration then forms between the opacity and limbus.
![]() The stroma progressively thins, usually over many years.
The stroma progressively thins, usually over many years.
![]() The peripheral edge of the gutter gently slopes, whereas the central edge is often steeper.
The peripheral edge of the gutter gently slopes, whereas the central edge is often steeper.
![]() Overlying epithelium remains intact. The gutter becomes more vascularied and wider over time.
Overlying epithelium remains intact. The gutter becomes more vascularied and wider over time.
![]() The lesion may eventually extend circumferentially or centrally. A yellow-white zone of lipid can be seen central to the advancing edge of the gutter.
The lesion may eventually extend circumferentially or centrally. A yellow-white zone of lipid can be seen central to the advancing edge of the gutter.
Two types of Terrien’s degeneration have been classified:
![]() The more common quiescent type is seen in older patients. These patients may be asymptomatic for a long time because the lesion produces no pain.
The more common quiescent type is seen in older patients. These patients may be asymptomatic for a long time because the lesion produces no pain.
![]() Inflammatory Terrien’s degeneration usually occurs in the younger age groups. These patients may have recurrent episodes of inflammation, episcleritis, or scleritis. This is treated with steroids.
Inflammatory Terrien’s degeneration usually occurs in the younger age groups. These patients may have recurrent episodes of inflammation, episcleritis, or scleritis. This is treated with steroids.
![]() Astigmatism may be produced from the marginal thinning. Typically, the lesion is superior, inducing against the rule astigmatism, which may be the presenting symptom. Astigmatism may be treated with glasses or contact lenses.
Astigmatism may be produced from the marginal thinning. Typically, the lesion is superior, inducing against the rule astigmatism, which may be the presenting symptom. Astigmatism may be treated with glasses or contact lenses.
Generally no treatment is required, unless perforation or impending perforation occurs. Initial conservative management for the severe astigmatism includes the use of spectacles or rigid gas-permeable contact lenses. Underlying corneal thinning should be monitored carefully
Credit: Cornea; Krachmer, Mannis & Holland. Photo credit: openeye._(insta)
Are you an Eye Professional? Register yourself in our Eye professional directory for Free.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.