Plateau iris syndrome
Plateau iris syndrome is a form of primary angle closure glaucoma caused by a large or anteriorly positioned ciliary body that leads to mechanical obstruction of trabecular meshwork.
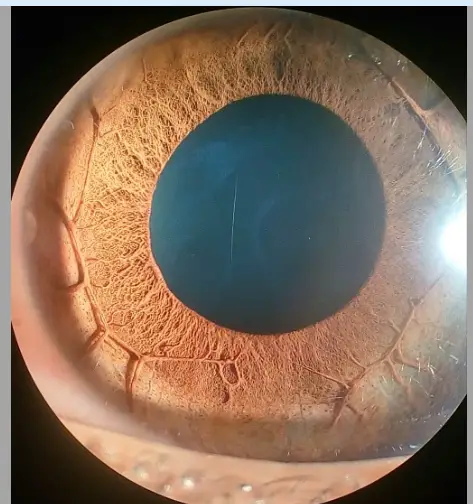
This mechanism is responsible for few (10%) atypical cases of acute angle closure glaucoma. Acute angle closure glaucoma associated with plateau iris is atypical in the patients that have normal central anterior chamber depth, flat iris plane and minimal pupillary block.
It has also been referred in the literature as an angle closure glaucoma without pupillary block. The anterior chamber angle is closed by a pushing mechanism because of the anterior positioned ciliary processes displacing the peripheral iris anteriorly. Such a situation is called plateau iris configuration and iridotomy is sufficient to control IOP in such patients.
Plateau iris syndrome is labeled when acute angle closure glaucoma occurs either spontaneously or after pharmacological dilation, in spite of patent iridotomy. Such eyes are treated with miotics and laser peripheral iridoplasty to produce thinning of the peripheral iris.
Symptoms of Plateau iris syndrome
The diagnosis of plateau iris is most commonly made in asymptomatic patients on routine examination of the eye. Patients with plateau iris tend to be female, in their 30-50s, hyperopic, and often have a family history of angle-closure glaucoma.
The condition should be suspected any time angle closure occurs in a younger patient, especially when the angle remains occludable after iridotomy. A symptomatic patient may initially present with headaches, eye pain, nausea, and vomiting – symptoms that are indicative of an acute rise in intraocular pressure. The patient may also complain of seeing halos around lights or blurry vision
Diagnosing of Plateau iris syndrome
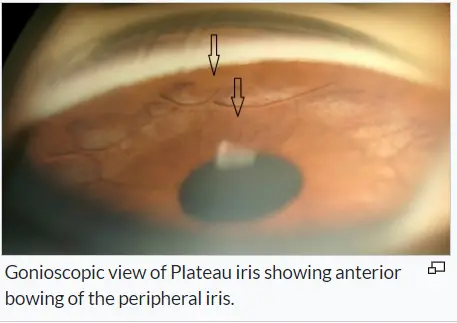
In addition to meticulous gonioscopic examination, the high resolution ultrasonic
biomicroscopy (UBM) examination and Anterior Segment OCT (AS-OCT) are very useful in
understanding the pathogenesis of primary angle closure disease.
These investigations are particularly useful in the documentation of plateau iris configuration, plateau iris syndrome, phacomorphic mechanism and post peripheral iridectomy angle dynamics.
Patients with plateau iris syndrome can be recognized by the lack of response in angle opening after iridotomy.
Prognosis of Plateau iris syndrome
Plateau iris is an ocular condition that requires appropriate diagnosis and treatment in order to prevent vision loss. Early recognition and intervention are key components to a good overall prognosis in this patient population.
Since patients with PIC often have an element of pupillary block, peripheral laser iridotomy is the first surgical intervention performed. A peripheral iridotomy, however, does not change the anatomy of the anterior chamber, so some patients with PIC may still experience a glaucoma crisis.
This situation most often occurs in patients with incomplete PIS who develop peripheral anterior synechiae and synechial angle closure. An acute glaucoma crisis after peripheral iridotomy is diagnostic for PIS. This acute crisis usually happens in the post-procedure period, but may also occur years later. Therefore, patients should undergo regular evaluation by an ophthalmologist after the procedure.
Treatment
Such eyes are treated with miotics and argon laser peripheral iridoplasty to produce thinning of the peripheral iris.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.