Hypertensive Retinopathy
Hypertensive retinopathy (HR) occurs when the retinal vessels get damaged due to elevated blood pressure.
Hypertensive retinopathy refers to fundus changes occurring in patients suffering from systemic
hypertension. Although the term hypertensive retinopathy implies only retinal changes but in
fact the clinical presentation includes changes of hypertensive:
- Retinopathy,
- Choroidopathy, and
- Optic neuropathy.
Epidemology:
The severity and duration of hypertension are directly proportional to the incidence of hypertensive retinopathy
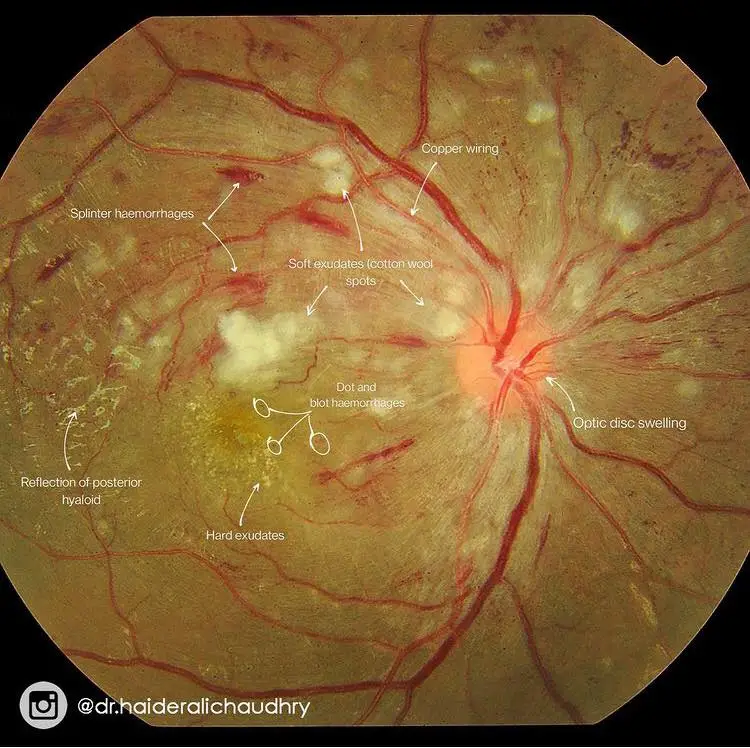
Image credit on Pic
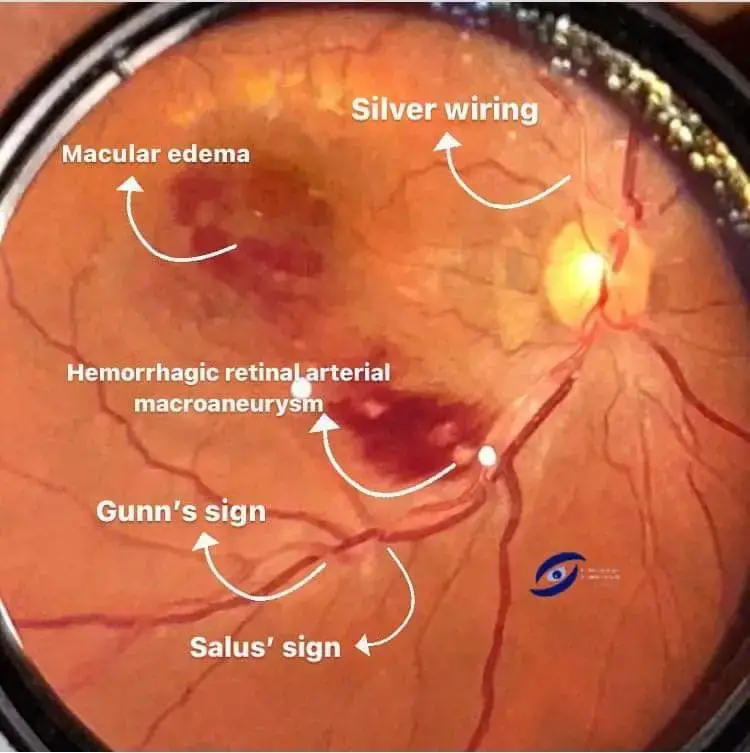
AV Crossing Changes
- Salus’s sign: Deflection of retinal vein as it crosses the arteriole.
- Gunn’s sign: Tapering of the retinal vein on either side of the AV crossing.
- Bonnet’s sign: Banking of the retinal vein distal to the AV crossing.
Gunn’s sign and salus sign in Hypertensive retinopathy.
Arterial Changes
- Decrease in the arteriovenous ratio to 1:3 ( the normal ratio is 2:3).
- Change in the arteriolar light reflex (light reflex appears as copper and/or silver wiring)
Also see: Optic disc and neuro retinal rim photographs
Retinal Changes
- Retinal hemorrhages:
- Dot-blot hemorrhages: Bleeding in the inner retinal layer
- Flame shaped hemorrhage: Bleeding is in the superficial retinal layer
- Retinal exudates:
- Hard exudates: Lipid deposits in the retina
- Soft exudates: These are also known as cotton wool spots which appear due to ischemia of the nerve fibers
Macular Changes
Macular star formation due to deposition of hard exudates around the macula.
Optic Nerve Changes
Optic disk swelling (also known as hypertensive optic neuropathy)
Clinical types of Hypertensive Retinopathy
Clinically, the hypertensive fundus changes can be described as:
- Chronic hypertensive retinopathy, and
- Malignant or acute hypertensive retinopathy.
Chronic hypertensive retinopathy
Patients with chronic hypertensive retinopathy are usually asymptomatic. Clinical situations in which chronic hypertensive retinopathy occurs include:
- Hypertension with involutionary (senile) sclerosis When hypertension occurs in elderly patients (after
the age of 50 years) in the presence of involutionary sclerosis the fundus changes comprise augmented arteriosclerotic retinopathy. - Chronic hypertension with compensatory arteriolar sclerosis
This condition is seen in young patients with prolonged benign hypertension usually associated
with benign nephrosclerosis. The young arterioles respond by proliferative and fibrous changes in
the media (compensatory arteriolar sclerosis). Advanced fundus changes in these patients have
been described as ‘albuminuric or renal retinopathy
Malignant hypertensive retinopathy
Malignant hypertension is not a separate variety of hypertension, but is an expression of its rapid
progression to a serious degree in a patient with relatively young arterioles undefended by fibrosis.
Fundus picture is characterised by changes of acute hypertensive retinopathy, choroidopathy and optic
neuropathy
Grading of Hypertensive Retinopathy
Staging of Hypertensive Retinopathy
Several classification schemes have been described to stage hypertensive retinopathy. No classification
is clinically useful. A few popular classifications, are given below, just for their historical value.
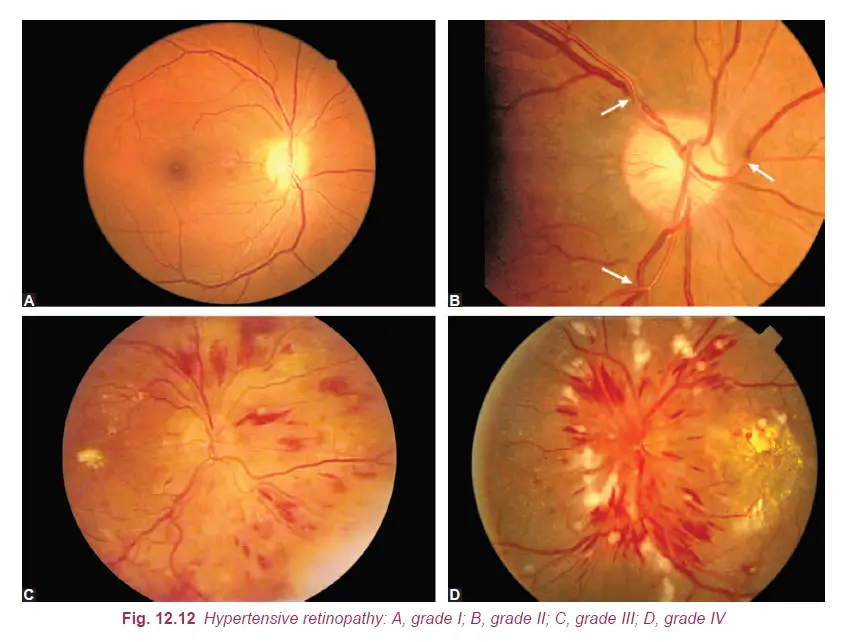
Keith and Wagner classification
- Grade I. Mild generalized arteriolar attenuation, particularly of small branches, with broadening
of the arteriolar light reflex and vein concealment(Fig. 12.12A). - Grade II. Marked generalized narrowing and focal attenuation of arterioles associated with deflection
of veins at arteriovenous crossings (Salus’ sign) (Fig. 12.12B). - Grade III. Grade II changes plus copperwiring of arterioles, banking of veins distal to
arteriovenous crossings (Bonnet sign), tapering of veins on either side of the crossings (Gunn
sign) and right-angle deflection of veins (Salu’s sign). Flame-shaped haemorrhages, cotton-wool
spots and hard exudates are also present (Fig. 12.12C). - Grade IV. All changes of grade III plus silver-wiring of arterioles and papilloedema (Fig. 12.12D).
Scheie classification of hypertensive Retinopathy
Staging of retinopathy changes is as follows:
- Stage 0. No visible retinal abnormalities
- Stage 1. Diffuse arteriolar narrowing; no focal constriction
- Stage 2. More pronounced arteriolar narrowing with focal constriction
- Stage 3. Focal and diffuse narrowing, with retinal haemorrhages
- Stage 4. Retinal oedema, hard exudates, optic disc edema
Management of Hypertensive Retinopathy
Mild hypertensive retinopathy requires blood pressure control only.
Moderate hypertensive retinopathy patients (characterised by retinal haemorrhages, microaneurysms, and cotton-wool spots) in addition to blood pressure control benefit from further assessment of vascular risk factors (e.g., cholesterol levels) and, if indicated, risk reduction therapy (e.g., cholesterol lowering agents).
Accelerated hypertensive retinopathy characterized by bilateral disk swelling which may occur in
conjunction with severe hypertension needing urgent antihypertensive management. In such instances,
physicians should aim for a small stepwise control of blood pressure over a few hours, and avoid a sudden reduction in blood pressure which may reduce perfusion of optic nerve head and central nervous
system (causing stroke).
Reference : (AK Khurana)
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.