Eales Disease: A Rare Retinal Disorder with Sight-Threatening Consequences
Eales disease, though rare, remains a significant cause of visual loss in young adults, especially males. It’s a condition that quietly progresses through distinct stages, leading to serious retinal damage and even blindness if not recognized early. Originally described by British ophthalmologist Henry Eales in 1880, this idiopathic condition continues to pose diagnostic and therapeutic challenges to ophthalmologists worldwide. Let’s explore what Eales disease is, how it affects the retina, and the treatment options available—alongside a unique case that breaks the typical pattern.
What is Eales Disease?
Eales disease is a rare, idiopathic inflammatory condition of the retina, specifically affecting the retinal veins (periphlebitis). It primarily targets the mid-peripheral retina and is characterized by:
Retinal periphlebitis (inflammation of peripheral retinal veins) Retinal capillary non-perfusion (ischemia) Retinal neovascularization (abnormal new vessel growth) Recurrent vitreous hemorrhage (bleeding into the eye’s vitreous cavity)
Though the exact cause is unknown, it is believed to have an autoimmune or hypersensitivity component, possibly related to tuberculosis antigen exposure.
Who is Affected?
Eales disease typically affects young males in their second or third decade of life. However, it can affect females aswell as illustrated by a case involving a 40-year-old female who presented to the emergency room with sudden vision loss. She was diagnosed with vitreous hemorrhage due to Eales disease, highlighting the need for broader awareness of this condition beyond its classic demographic.
The Three Stages of Eales Disease
Eales disease progresses through three distinct phases:
1. Inflammatory Stage (Early)
Characterized by periphlebitis of the peripheral and mid-peripheral retinal veins. Signs include venous dilation, perivascular exudates, and retinal inflammation. Multiple quadrants can be involved simultaneously.
2. Ischemic Stage (Intermediate)
As the disease progresses, capillary non-perfusion sets in. This stage is marked by arteriovenous shunts, venous beading, and microaneurysms. The retina shows a clear boundary between perfused and non-perfused areas.
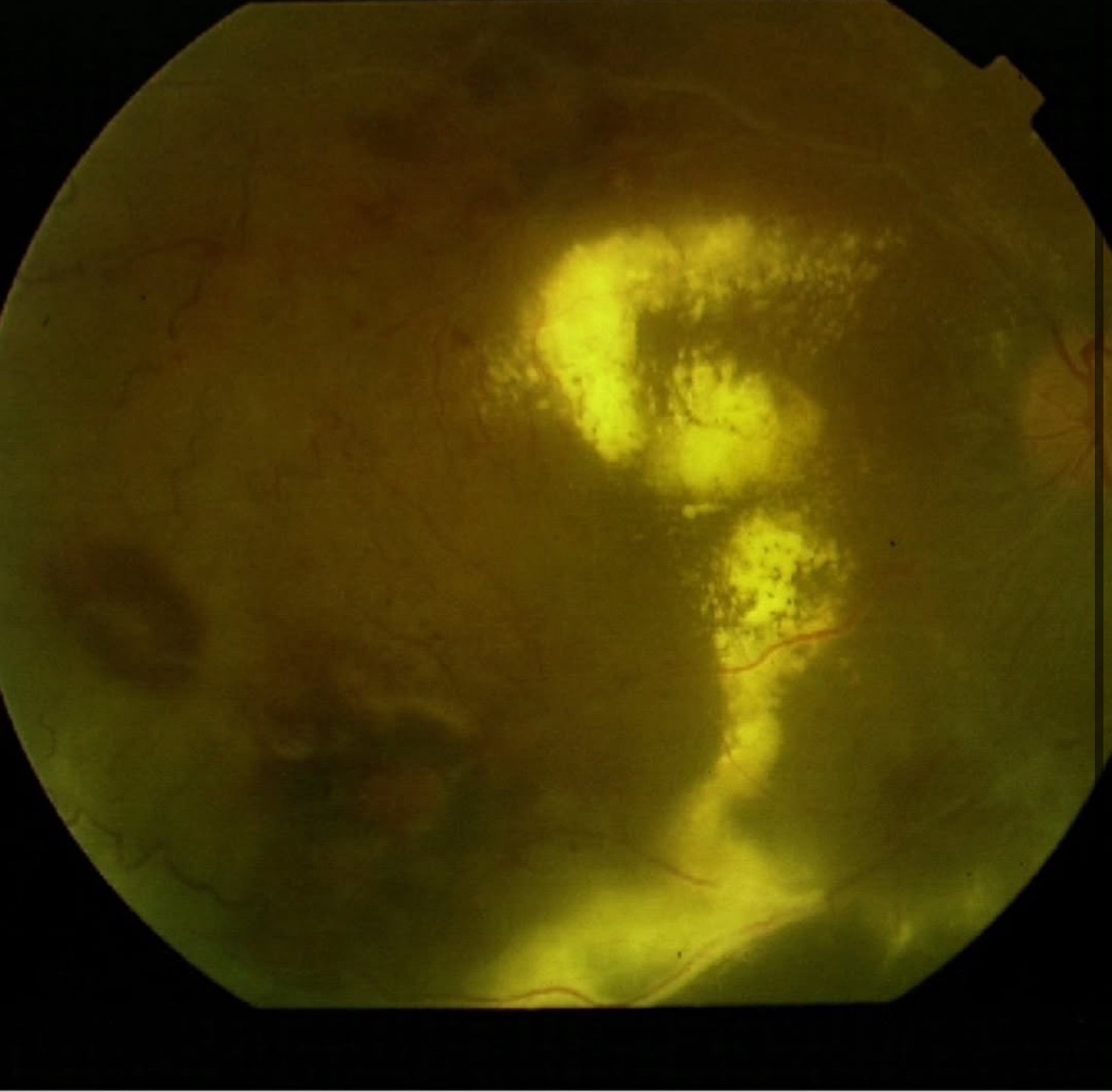
3. Proliferative Stage (Late)
In response to ischemia, neovascularization occurs at the junction of healthy and ischemic retina. These fragile new vessels often rupture, leading to recurrent vitreous hemorrhage. Complications include tractional retinal detachment, potentially causing permanent vision loss.
Case Study Highlight
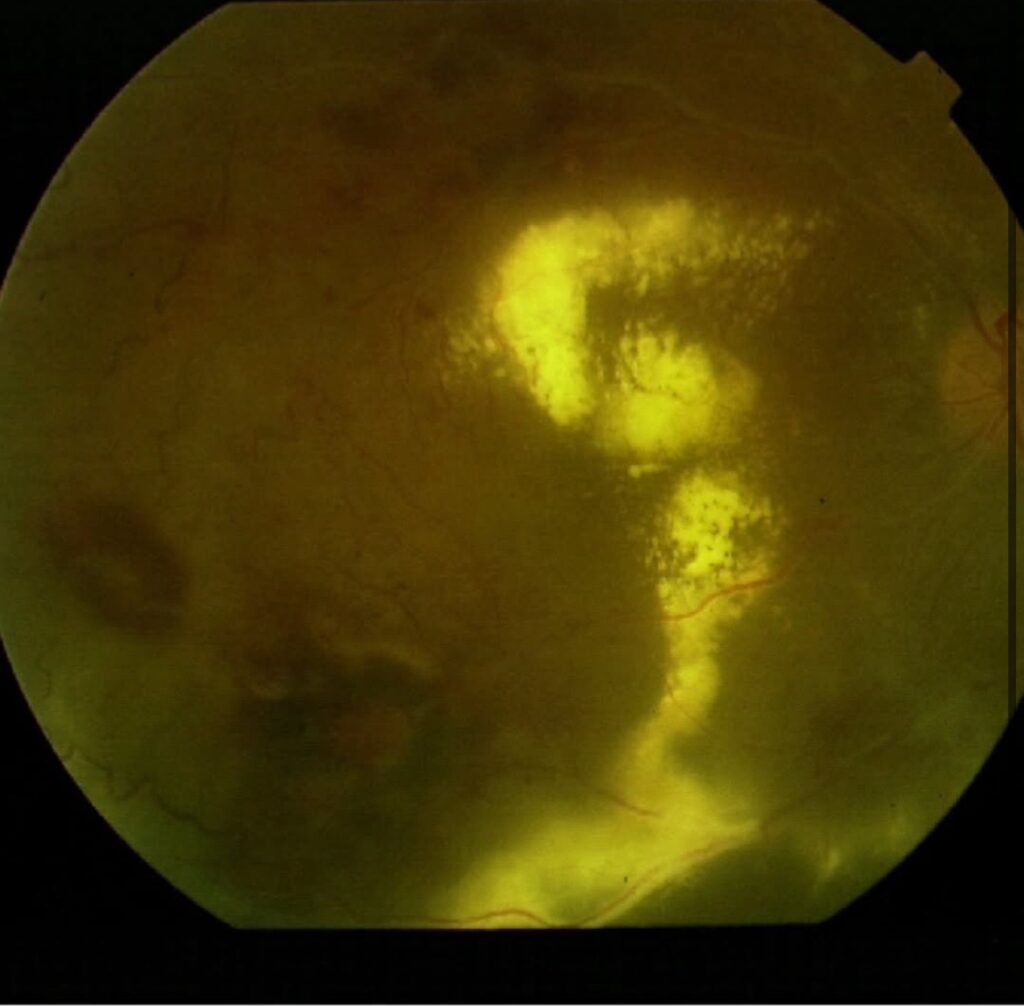

The patient in this case—shared by Dr. Gil Calvão-Santos—was a woman in her 40s who presented with sudden vision loss in the right eye. The examination revealed a vitreous hemorrhage, a hallmark of the proliferative stage of Eales disease. Interestingly, she had asymmetrical disease, with her right eye more severely affected, resulting in significantly reduced vision.
This case is notable not only for the patient’s age and gender, which are atypical for Eales disease, but also for the unilateral severity, underscoring how unpredictable the disease can be.
How is Eales Disease Diagnosed?
Diagnosis is primarily clinical but requires supportive imaging:
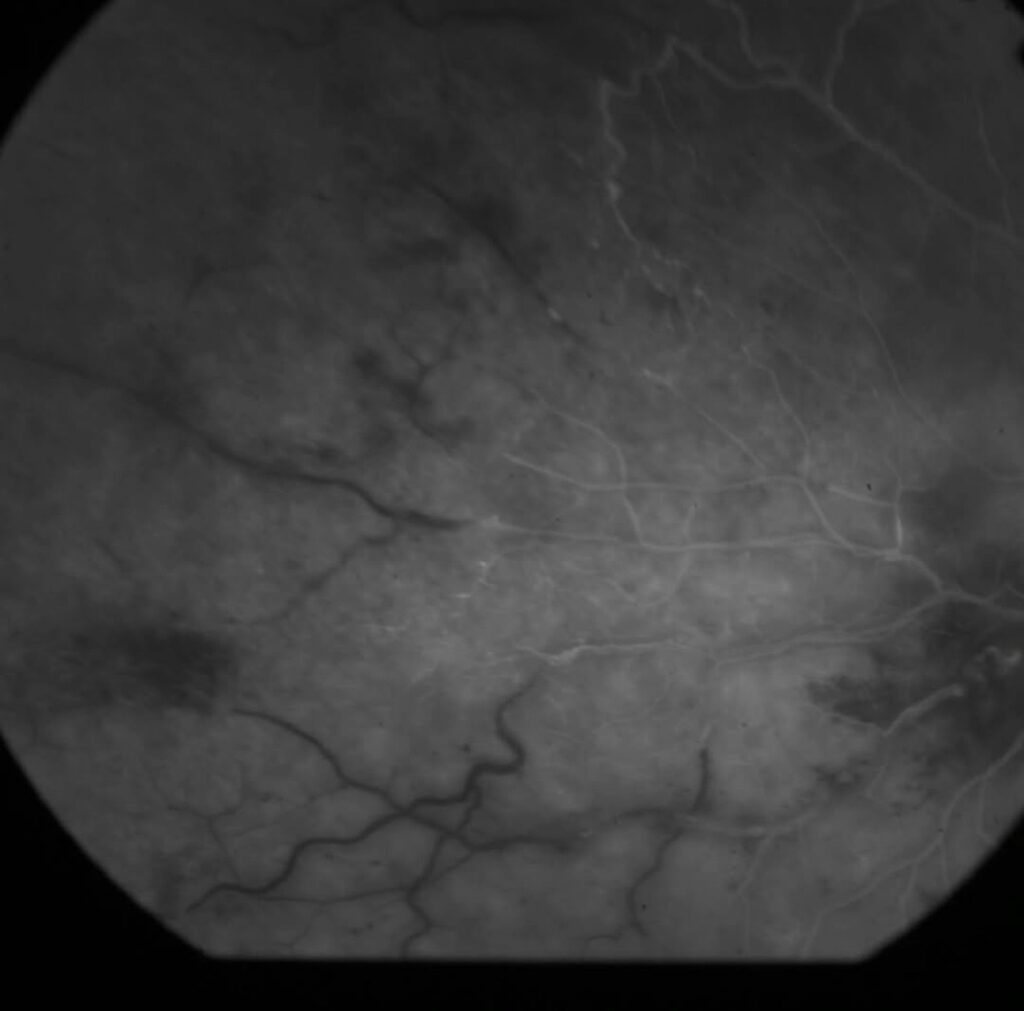
Fundus Examination: Reveals periphlebitis, ischemia, and neovascularization. Fluorescein Angiography: Essential for identifying capillary non-perfusion and neovascular areas. OCT (Optical Coherence Tomography): Can assess macular involvement and traction. B-scan Ultrasound: Used in cases with dense vitreous hemorrhage to rule out retinal detachment. Tuberculosis Screening: Though not directly caused by TB, hypersensitivity to TB protein is common.
Treatment Options for Eales Disease
Treatment depends on the disease stage:
1. Medical Management
Corticosteroids: To control inflammation in early stages. Anti-tubercular therapy: If latent or active TB is suspected. Immunosuppressive agents: For resistant or recurrent inflammation.
2. Laser Photocoagulation
Applied in ischemic areas to prevent neovascularization. Helps reduce the risk of recurrent vitreous hemorrhage.
3. Intravitreal Anti-VEGF Injections
Used in the proliferative stage to regress abnormal blood vessels. Often combined with laser therapy.
4. Vitrectomy Surgery
Necessary in cases of non-resolving vitreous hemorrhage or tractional retinal detachment. Removes the vitreous gel and clears blood to restore vision.
Prognosis
With timely diagnosis and treatment, the prognosis can be good. However, untreated Eales disease can lead to irreversible vision loss, especially when complicated by retinal detachment or macular traction. Regular follow-up is crucial to monitor disease progression and prevent recurrence.
Types of Retinal Hemorrhages and its treatment.
Conclusion
Eales disease, though uncommon, is a serious retinal condition that demands prompt recognition and intervention. The case of a 40-year-old female with sudden vision loss serves as a vital reminder that this disease is not exclusive to young males. Understanding the three progressive stages and the available treatment options is essential for preserving sight and improving quality of life in affected individuals.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.