10 Common Questions About Applanation Tonometry Answered
1. What is Applanation Tonometry?
Applanation Tonometry is a method used to measure intraocular pressure (IOP) by flattening a specific area of the cornea. It is the gold standard for IOP measurement, particularly with the Goldmann tonometer, which is commonly used in clinical settings.
2. How does Applanation Tonometry work?
The technique is based on the principle that the pressure inside the eye equals the external force applied to flatten the cornea divided by the area of flattening. The Goldmann tonometer measures the force needed to flatten a 3.06 mm diameter area on the cornea.
Goldman Applanation tonometry Principle:
Goldman applanation tonometry is based upon the Imbert-Fick principle: such that the IOP measurement can be determined by the amount of force needed to flatten a fixed area of cornea. We push on the eye with the blue-light applanator trying to flatten a round cornea surface with a diameter of 3.06 mm (that’s the area that the variable-force scale is callibrated for).
3. Why is the diameter of 3.06 mm used in Applanation Tonometry?
The 3.06 mm diameter is used because it cancels out the opposing forces from corneal rigidity and tear film surface tension, providing an accurate IOP measurement.
What is Imbert Fick law?
The pressure inside a sphere (P) is equal to External force (F) needed to flatten a portion of a sphere divided by the area of sphere (A).
P = F/A
P= Pressure F= Force A= Area
Based on Imbert Fick Law Commonly used applanation tonometers are as follows
- Goldmann applanation tonometer
- Perkin’s applanation tonometer
- Pneumatic tonometer
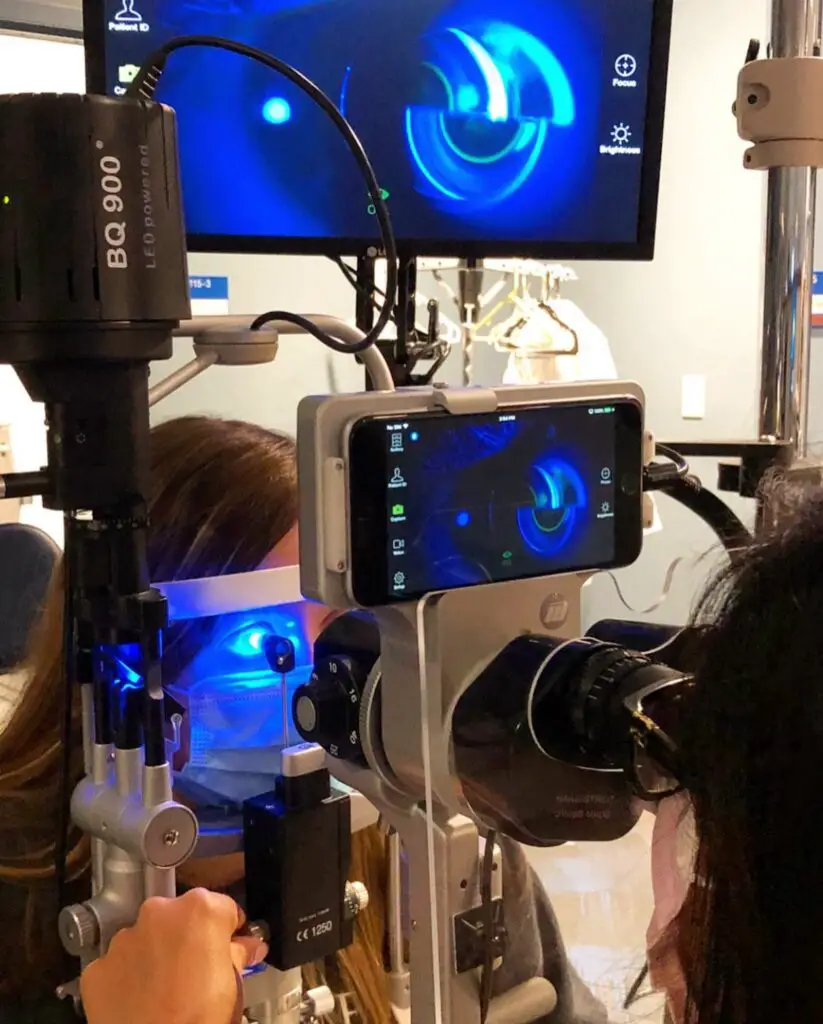
Applanation Tonometer
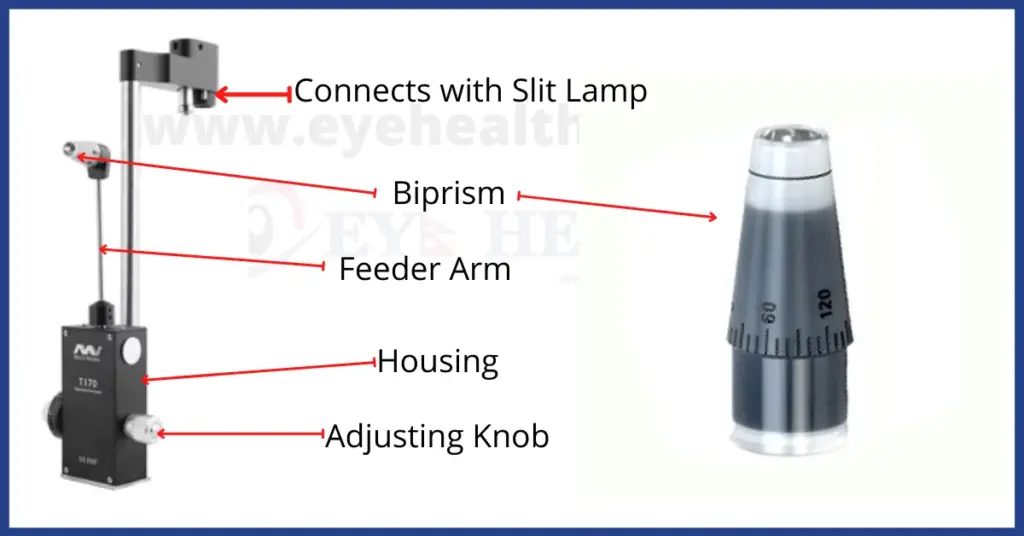
Preparation
First of all, prism needs to be disinfected with isopropyl alcohol 70%. Make it dry by wiping prism with a dry clean swab. Check that the gradation marked ‘0’ on the measuring prism is aligned with the white marker point on the tonometer head remember that adjusting the tonometer prism is done on patients with significant astigmatism. Check that the calibrated dial of the tonometer is set around 10 mmHg. Set the magnification of the slit lamp at 10X. The Goldmann tonometer should be regularly calibrated.
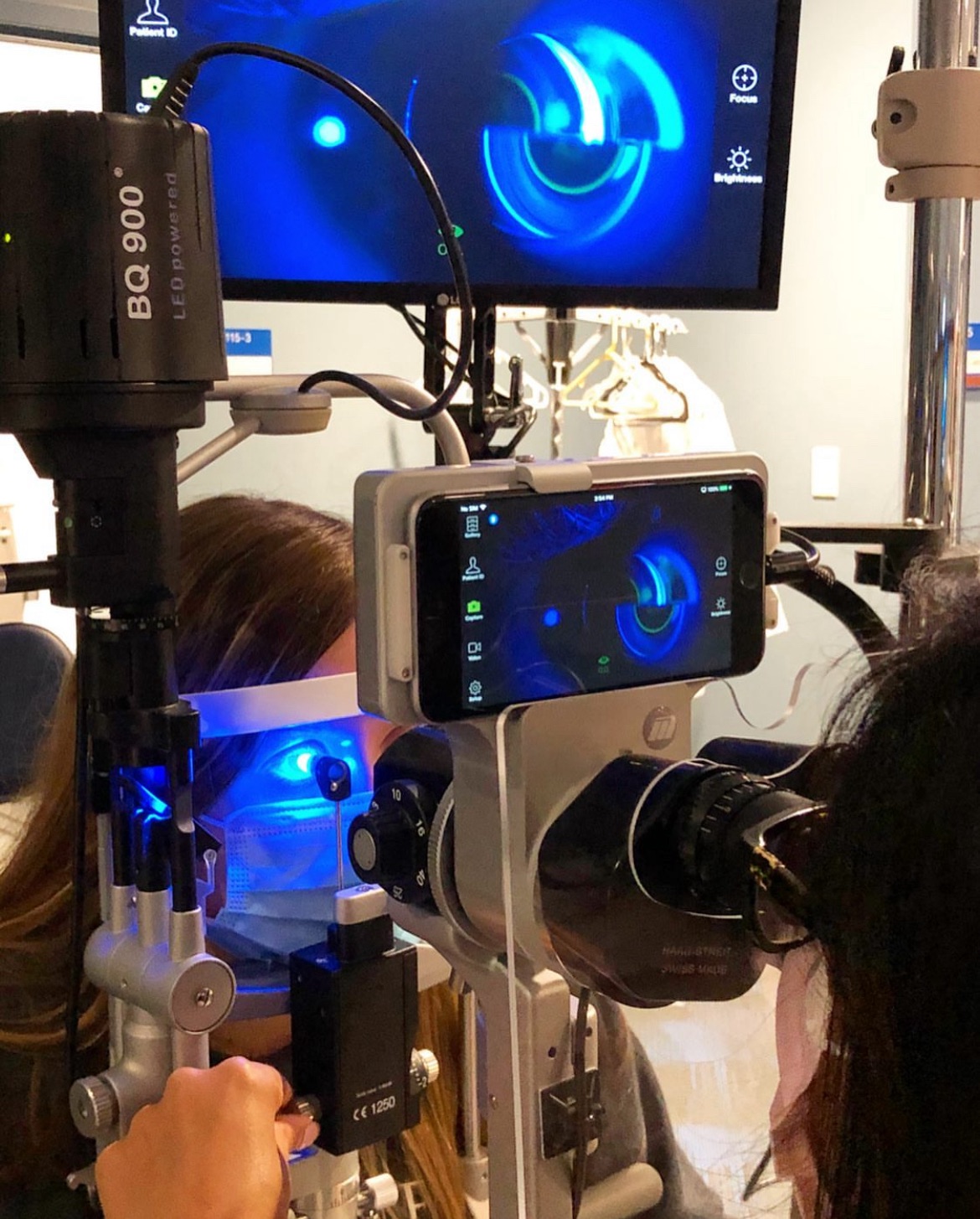
Procedure to Measure Intraocular Pressure
- Instil the local anaesthetic drops eg Lignocaine 4% or Proparacaine
- Apply fluorescein strip
- For measuring the IOP in the right eye, make sure the slit beam is shining onto the tonometer head from the patient’s right side; for the left eye, the beam should come from the patient’s left side.
- Move the filters so that the cobalt blue filter.
- Make wide beam and full brightness to make it easy for visualising the fluorescein semi-circles easier
- Instruct the patient to look straight ahead, open both eyes wide, and ask not to move eyes in any direction.
- With the thumb, gently hold up the patient’s top eyelid, taking care not to put any pressure on the eye
- Direct the blue light from the slit lamp onto the prism head. Make sure that the tonometer head is perpendicular to the eye.
- Move the tonometer forward slowly until the prism rests gently on the centre of the patient’s cornea.
- With the other hand, turn the calibrated dial on the tonometer forward until the two fluorescein semi-circles in the prism head are seen to meet and form a horizontal ‘S’ shape. The correct end point is when the inner edges of the two fluorescein semi-circle images just touch as shown in the image below.
Goldman Applanation Mires for Glaucoma
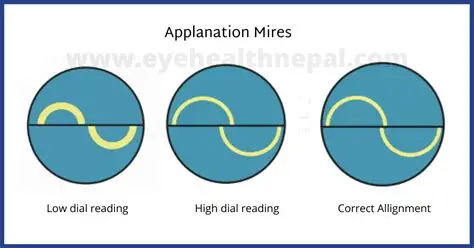
credit-eyehealthnepal.com
Note the reading on the dial and record it in the notes. The recorded intraocular pressure
is determined by multiplying the dial reading by ten.
4. Is Applanation Tonometry painful?
No, Applanation Tonometry is not painful. The procedure typically involves numbing the eye with anesthetic drops to ensure comfort during the measurement.
5. What factors can affect the accuracy of Applanation Tonometry?
Factors such as central corneal thickness, corneal edema, scarring, or irregularities can influence the accuracy of the IOP readings, potentially leading to underestimation or overestimation of the true pressure.
6. What is the normal range for intraocular pressure (IOP)?
The normal range for IOP is typically between 10 and 21 mmHg. Readings outside this range may indicate potential eye conditions, such as glaucoma
7. How often should IOP be measured?
For individuals at risk of glaucoma or other eye conditions, IOP should be measured regularly as part of routine eye exams. The frequency can vary based on personal risk factors and the recommendation of an eye care professionals
8. Can Applanation Tonometry detect glaucoma?
While Applanation Tonometry is an essential tool for measuring IOP, which is a risk factor for glaucoma, it is not a definitive diagnostic tool for glaucoma. Other tests are needed to diagnose glaucoma accurately.
9. What are the limitations of Applanation Tonometry?
Limitations include its dependence on corneal properties, such as thickness and rigidity, which can affect accuracy. It also requires patient cooperation and proper technique by the examiner.
10. How does Applanation Tonometry compare to other methods of measuring IOP?
Applanation Tonometry is considered the gold standard due to its accuracy and reliability. However, other methods like non-contact tonometry (air-puff test) and rebound tonometry are also used, each with its advantages and limitations.
Follow us in Facebook
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.