Iridocorneal Endothelial (ICE) Syndrome: A Practical Guide for Optometrists
Among the many conditions that mimic glaucoma, Iridocorneal Endothelial (ICE) syndrome stands out for its complexity and clinical challenges.
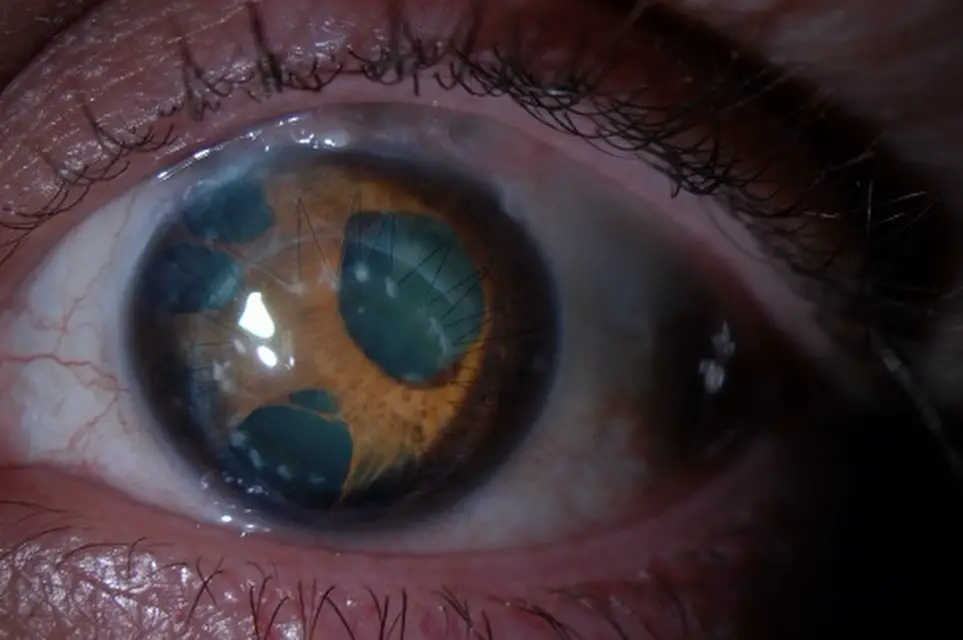
It is rare, usually unilateral, and progressive, presenting with a triad of abnormal corneal endothelium, iris changes, and secondary angle-closure glaucoma.
For optometrists, recognizing the signs of ICE is vital, since early suspicion and referral can preserve vision and guide patients toward timely intervention.
Understanding ICE Syndrome
ICE syndrome occurs when corneal endothelial cells transform into “ICE cells” with epithelial-like characteristics. These cells proliferate and migrate across the angle and iris, laying down a membrane that contracts, distorting the pupil and causing peripheral anterior synechiae (PAS). The corneal pump mechanism weakens, resulting in edema, while progressive angle closure leads to glaucoma.
Clinical Variants
ICE syndrome is classified into three overlapping subtypes:
Chandler syndrome – prominent corneal endothelial changes and edema; iris changes are subtle. Progressive iris atrophy – striking iris thinning, corectopia (displaced pupil), and polycoria (multiple pupils). Cogan-Reese syndrome – iris nodules or diffuse pigmented lesions with aggressive glaucoma.
Each variant shares the same pathophysiology but differs in clinical presentation and severity.
Clinical Examination: What Optometrists Should Look For
History: Unilateral blurred vision, halos, pain from IOP spikes, or longstanding changes in pupil shape.
Slit-lamp findings:
Cornea: “hammered silver” or beaten bronze endothelium. Iris: corectopia, holes, or nodules depending on subtype. Anterior chamber: PAS visible on gonioscopy.
Investigations:
IOP measurement (often fluctuating, can be high).
Gonioscopy to assess PAS extent. Specular microscopy (reveals ICE cells).
Anterior segment OCT/UBM for synechiae and angle closure.
Visual field and OCT RNFL for glaucoma staging.
Differential Diagnosis
ICE syndrome must be distinguished from conditions with overlapping features:
Posterior polymorphous corneal dystrophy (PPCD): usually bilateral, hereditary, and less iris involvement.
Axenfeld-Rieger anomaly: congenital, systemic associations.
Fuchs’ endothelial dystrophy: bilateral, guttata, morning blur.
Herpetic endotheliitis: inflammation, keratic precipitates, corneal anesthesia.
Management Strategies
There is no cure for ICE syndrome; treatment focuses on controlling intraocular pressure (IOP) and managing corneal complications.
Glaucoma Management
Topical aqueous suppressants (beta-blockers, CAIs, alpha-agonists) are first-line. Laser trabeculoplasty (ALT/SLT) is ineffective and usually avoided due to endothelial membrane blockage.
Surgical options include trabeculectomy with antimetabolites or glaucoma drainage devices (often preferred due to higher success rates).
Corneal Disease
Early edema: treated with hypertonic saline (5%) and hair-dryer technique.
Advanced edema: scleral or bandage contact lenses for comfort.
Keratoplasty (DSAEK/DMEK/PK): indicated for decompensated corneas, though graft survival may be limited due to recurrence of ICE changes.
Iris and Cosmetic Issues
Corectopia and polycoria causing glare or cosmetic concerns may be managed with tinted or prosthetic contact lenses.
Optometric Role and Referral
Optometrists play a frontline role in:
Identifying suspicious unilateral glaucoma with corneal and iris changes. Documenting corneal and iris appearance with slit-lamp photos. Avoiding inappropriate referrals for SLT. Referring early to glaucoma and cornea specialists with detailed findings.
Sample referral note:
“Unilateral ICE syndrome suspected (Chandler type). Hammered silver endothelium with mild stromal edema; corectopia noted; PAS from 3–6 o’clock on gonioscopy; IOP 26 mmHg. RNFL OCT shows inferior thinning. Started on topical beta-blocker. Request glaucoma and cornea opinion.”
Prognosis
The long-term visual outcome depends on glaucoma control and corneal clarity. Patients should be counseled about the likelihood of multiple procedures over time and the chronic, progressive nature of the condition.
Further Reading
EyeWiki: Iridocorneal Endothelial Syndrome StatPearls: ICE Syndrome Overview Review of Ophthalmology – ICE Syndrome
Conclusion
ICE syndrome is a rare yet important condition for optometrists to recognize. Its unique combination of endothelial abnormalities, iris changes, and secondary glaucoma demands vigilance and informed co-management. By identifying the early signs, documenting carefully, and referring appropriately, optometrists play a crucial role in preventing irreversible vision loss in these patients.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.