Understanding Optic Disc Abnormalities
Have you ever wondered how your eyes relay the world to your brain? The optic disc—a tiny but powerful structure in the back of your eye—is the critical hub where visual information begins its journey. But what happens when this vital nerve center is disrupted?
Optic disc abnormalities, ranging from congenital defects to acquired conditions, can impact vision profoundly. They often go unnoticed until symptoms like blurred vision or visual field loss appear, making early detection crucial. Thanks to modern diagnostic advancements like Optical Coherence Tomography (OCT), we’re now better equipped to understand and manage these conditions.
In this article, we explore the fascinating world of optic disc abnormalities, their causes, effects on visual acuity, and how eye care professionals diagnose and treat these complex conditions. Stay with us to uncover insights that might just change the way you think about eye health!
Understanding Canine Retinal Detachment
What are Optic disc abnormalities?
Optic disc abnormalities are structural or functional issues of the optic nerve head that significantly impact vision. The optic disc is the entry point of the optic nerve into the retina, playing a pivotal role in transmitting visual signals to the brain. Abnormalities in the optic disc can arise from congenital conditions, structural anomalies, or disease processes, leading to vision impairment or loss.
Congenital Abnormalities
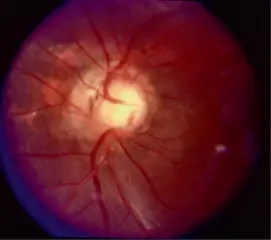
Morning Glory Syndrome (MGS)

A rare congenital anomaly characterized by a funnel-shaped optic disc surrounded by retinal pigment epithelium disturbances.
- Symptoms: Reduced vision, strabismus, and occasionally systemic associations like basal encephalocele.
- Diagnosis: Fundoscopic examination and OCT imaging are vital tools for identification
Morning Glory Syndrome (MGS) is a congenital anomaly of the optic disc characterized by its distinctive funnel-shaped excavation. The optic nerve head is enlarged, with a surrounding area of pigmentation that resembles the radiating petals of a morning glory flower. This condition is often unilateral and may be associated with other ocular or systemic abnormalities, such as transsphenoidal basal encephalocele or midline cranial defects.
findings:
- Funnel-shaped disc excavation: The optic disc appears deeply cupped with a central glial tuft.
- Enlarged optic nerve head: The optic disc is larger than normal, often with irregular margins.
- Radial blood vessel configuration: Retinal vessels spread out from the center in a spoke-like arrangement.
- Surrounding chorioretinal pigment changes: These often appear as a ring or a halo surrounding the disc.
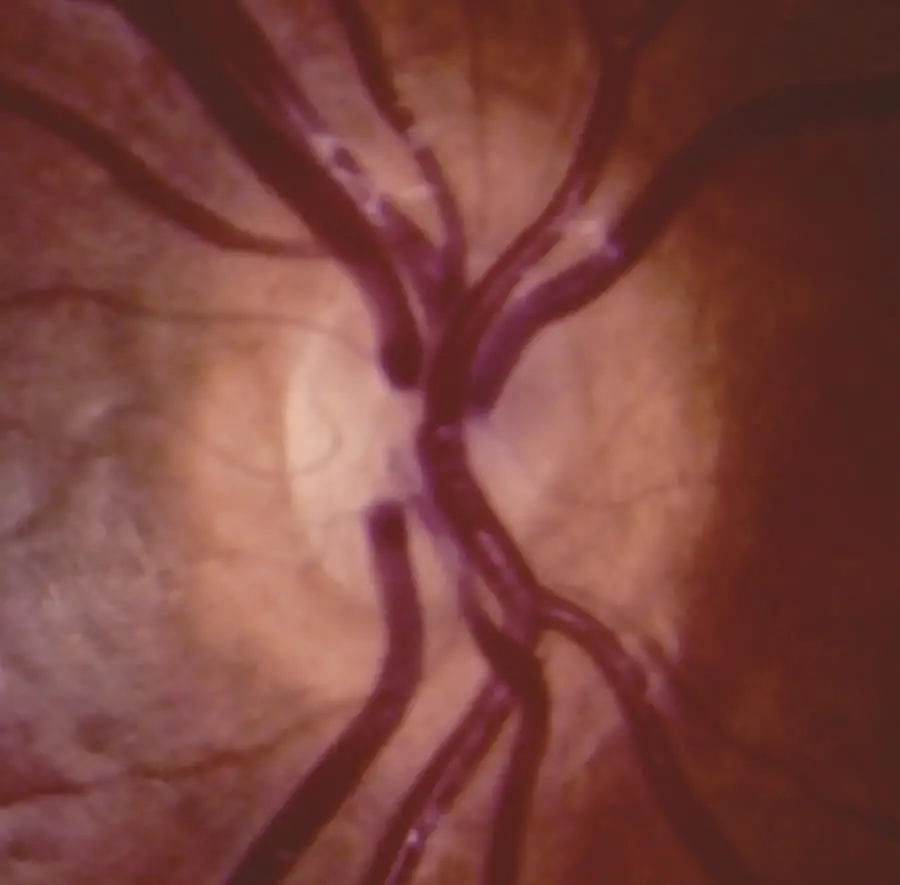
Optic Disc Coloboma
A developmental defect caused by incomplete closure of the embryonic fissure, resulting in a malformed optic nerve.
What is Optic Disc Coloboma?
Optic disc coloboma is a congenital anomaly resulting from incomplete closure of the embryonic fissure during eye development. This leads to an excavation in the optic nerve head that may involve adjacent structures such as the retina and choroid. The condition typically manifests as a white, glistening excavation in the optic disc, often accompanied by visible changes in the surrounding retina and blood vessels.
- Appearance: The optic disc appears enlarged with a bowl-shaped excavation, usually involving the inferior portion. The base of the coloboma may extend to the adjacent retina and choroid.
- Systemic Associations: This anomaly can occur in isolation or as part of syndromes like CHARGE (coloboma, heart defects, choanal atresia, growth retardation, genital abnormalities, and ear anomalies).
- Visual Impact: Vision can range from normal to significantly impaired, depending on the extent of the anomaly and associated complications such as retinal detachment or serous maculopathy.
Optic Nerve Hypoplasia (ONH)
Image
Involves underdevelopment of the optic nerve.
- Clinical Features: Small optic disc with reduced or absent central vision.
- Systemic Links: Often associated with midline brain anomalies and endocrine dysfunction
Optic Nerve Hypoplasia (ONH) is a congenital anomaly characterized by the underdevelopment of the optic nerve, often resulting in reduced visual acuity and a spectrum of associated systemic anomalies. This condition is a leading cause of childhood visual impairment and presents with significant variability in its clinical and functional impact.
Clinical Features
ONH typically manifests as a small, pale optic disc surrounded by a “double-ring sign,” where an inner ring represents the underdeveloped optic nerve and an outer ring reflects the surrounding sclera. Visual acuity can range from normal to severe impairment, with bilateral cases often associated with more profound deficits. Other ocular findings may include strabismus, nystagmus, and reduced visual fields, depending on the extent of the hypoplasia.
Acquired Optic Disc Disorders
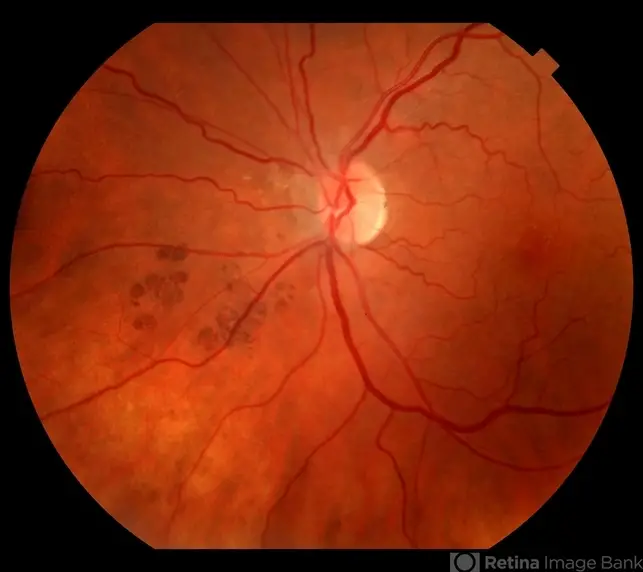
Papilledema

Swelling of the optic nerve head due to increased intracranial pressure.
- Primary Causes: Tumors, trauma, or idiopathic intracranial hypertension.
- Symptoms: Transient visual obscurations, headaches, and nausea.
- Management: Treating the underlying cause is crucial to prevent permanent vision damage
- What is Papilledema?
Papilledema refers to the swelling of the optic nerve head due to increased intracranial pressure (ICP). Unlike other optic nerve anomalies, it is not a primary disorder of the eye but a secondary response to pressure transmitted to the optic nerve via the subarachnoid space. Papilledema is a critical finding that necessitates immediate investigation for underlying causes, such as intracranial masses, hydrocephalus, or idiopathic intracranial hypertension (IIH).
Glaucomatous Optic Neuropathy
Chronic progressive damage caused by elevated intraocular pressure (IOP).
- Key Findings: Optic disc cupping and thinning of the retinal nerve fiber layer.
- Diagnosis: OCT and visual field testing are gold standards
Optic Disc Drusen
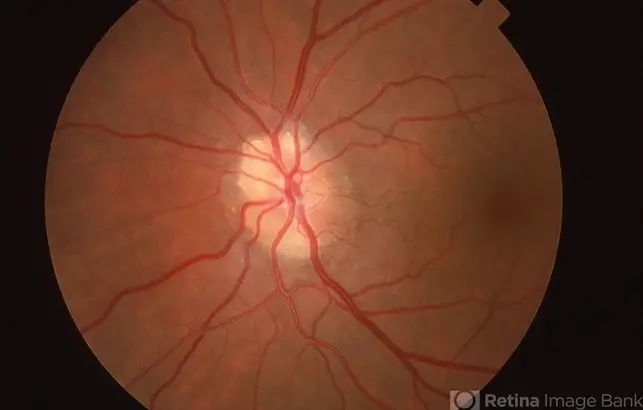
Image –Drusen of optic nerve
Calcified deposits within the optic nerve head.
- Symptoms: Often asymptomatic but can cause visual field loss over time.
- Diagnosis: Ultrasonography and autofluorescence imaging are essential diagnostic tools
Optic Neuritis: Inflammation of the optic nerve, often associated with autoimmune diseases like multiple sclerosis (MS) or neuromyelitis optica
Secondary to Systemic Diseases
Diabetic Optic Neuropathy: Chronic diabetes can lead to vascular damage affecting the optic nerve.
Hypertensive Retinopathy: Uncontrolled hypertension may cause swelling or atrophy of the optic disc.
The diagnostic approach
The diagnostic approach to papilledema involves a combination of history-taking, clinical examination, advanced imaging, and systemic evaluation. A thorough review of symptoms such as persistent headaches, transient visual obscurations, nausea, or pulsatile tinnitus is crucial to assess for signs of increased intracranial pressure (ICP). During ophthalmoscopy, examine the optic disc for hyperemia, blurred margins, absence of the optic cup, and associated findings like peripapillary hemorrhages.
Advanced imaging techniques provide significant insight. Optical Coherence Tomography (OCT) allows for detailed measurement of the retinal nerve fiber layer (RNFL) thickness, identifying structural changes due to disc swelling. Fundus autofluorescence (FAF) is particularly useful for distinguishing papilledema from optic disc drusen. Visual field testing aids in assessing functional damage, highlighting abnormalities like enlarged blind spots or peripheral constriction. Neuroimaging, including MRI or MRV, is essential to rule out intracranial masses, venous sinus thrombosis, or other structural anomalies contributing to increased ICP.
Systemic workup includes monitoring blood pressure to exclude hypertensive causes and performing lumbar puncture to measure cerebrospinal fluid (CSF) pressure and analyze for infections or inflammatory conditions. The integration of high-resolution imaging techniques like OCT and FAF has revolutionized the management of optic nerve disorders, enabling early detection and precise differentiation between papilledema and mimicking conditions. Early and accurate diagnosis ensures appropriate intervention to prevent permanent optic nerve damage and vision loss.
Optic Disc Abnormalities Influence on Visual Acuity
The impact of optic disc abnormalities on vision depends on the underlying condition and its progression:
- Congenital Conditions often lead to structural changes resulting in irreversible vision loss.
- Acquired Disorders, such as papilledema or glaucoma, can cause progressive vision loss if untreated but may stabilize with timely intervention.
- Optic Disc Drusen may remain asymptomatic but predispose patients to subtle visual field deficits
Management Strategies of Optic Disc Abnormalities
Management of optic disc abnormalities is multidisciplinary, involving:
- Medical Management: Corticosteroids for inflammatory conditions like optic neuritis.
- Surgical Interventions: Necessary in severe cases like optic nerve sheath fenestration for papilledema.
- Regular Monitoring: Imaging and functional assessments to monitor disease progression
Referral Guidelines
- For congenital anomalies, monitor visual function and educate patients about potential complications.
- In cases of papilledema, urgent referral to neurology or neurosurgery is critical.
- For optic disc drusen, provide reassurance but monitor for associated visual field defects
Conclusion
The optic disc serves as the gateway for the retinal nerve fibers into the brain, playing a central role in vision. Abnormalities of the optic disc, whether congenital or acquired, can lead to significant visual impairment or loss. Understanding these conditions’ diagnostic evolution and influence on visual acuity is crucial for effective treatment and management
Optic disc abnormalities present unique diagnostic and therapeutic challenges. Advances in imaging and a deeper understanding of their pathophysiology have enhanced early detection and personalized management approaches. Timely intervention remains critical to preserving vision and improving patient outcomes.
Reference
https://pubmed.ncbi.nlm.nih.gov/21601065
Image credit-https://imagebank.asrs.org/
