Five-Step Approach to Visual Field Interpretation
Interpreting a visual field test is a crucial skill for optometrists and ophthalmologists. One of the most common mistakes in visual field interpretation is jumping to a global evaluation without thoroughly analyzing detailed patterns of visual field loss. To ensure a systematic approach, we suggest following a simple five-step process for accurate visual field interpretation.
1. Determine if the Visual Field is Normal or Abnormal
The first step is to evaluate each eye separately to determine whether the visual field is normal or abnormal. Automated perimetry results assist in this process by providing both point-by-point and summary comparisons of the patient’s test results against age-matched normative values. If both eyes show normal results in both statistical comparison and clinical assessment, further evaluation is unnecessary.
2. Assess Testing Conditions and Artifacts
If an abnormality is detected, examine ancillary information to confirm proper test conditions. Verify that the appropriate near correction was used, the pupil size was adequate, and the patient’s fixation was stable. Consider potential nonpathologic causes such as lens rim artifacts, ptosis, fatigue, or drowsiness, as these can falsely indicate visual field loss. If necessary, consult the technician to gather additional insights about the patient’s condition during testing.
3. Determine If the Defect Is Monocular or Binocular
Identifying whether the abnormality affects one or both eyes is key to localizing the defect:
- Monocular defects typically indicate a disorder anterior to the optic chiasm.
- Binocular defects suggest involvement at or posterior to the chiasm, or bilateral intraocular or optic nerve disease.
Mastering Automated Perimetry: Essential Tips and Tricks.
4. Identify the General Location of the Visual Field Loss
Each eye should be assessed independently to determine whether the defect is located in the superior, inferior, nasal, temporal, or central visual field. Understanding the pattern of loss can help localize the lesion:
- Bitemporal hemianopia (respects the vertical midline) suggests chiasmal pathology.
- Homonymous hemianopia (nasal defect in one eye, temporal defect in the other) points to retrochiasmal lesions.
- Binasal defects or isolated nasal loss may indicate glaucoma or optic neuropathies.
- Central scotomas often suggest macular disorders.
5. Analyze the Specific Shape, Patterns, and Features
Finally, examine the characteristics of the visual field defect:
- Does it respect the horizontal or vertical meridian?
- Is the shape arcuate, circular, pie-shaped, or irregular?
- In binocular defects, is the field loss congruous (symmetric) or incongruous (asymmetric)?
- Are the edges of the defect steep or gradual?
By following these five steps, practitioners can systematically analyze visual field results, reducing errors and ensuring accurate localization of visual pathway abnormalities. This structured approach enhances diagnostic accuracy and aids in formulating appropriate management strategies for patients.
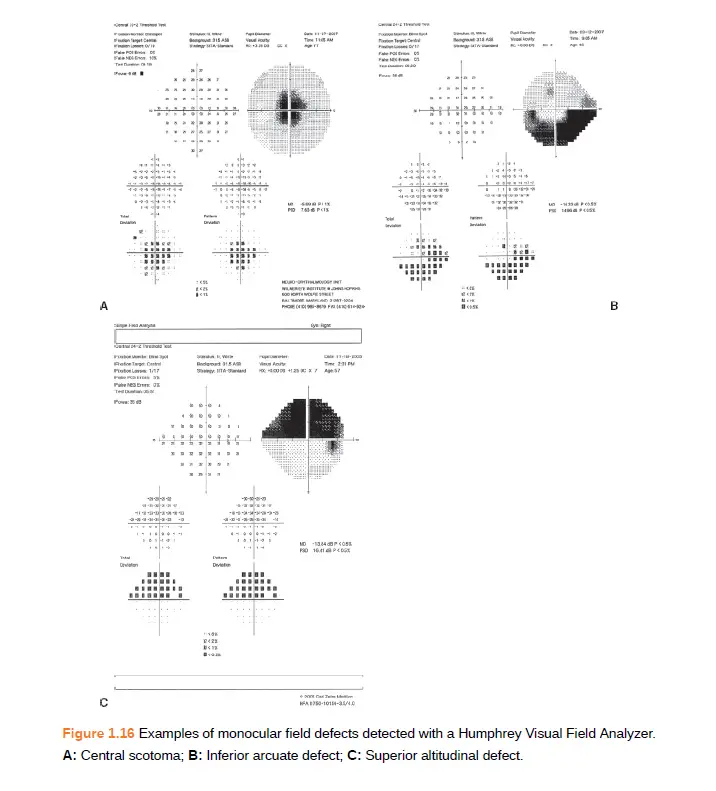
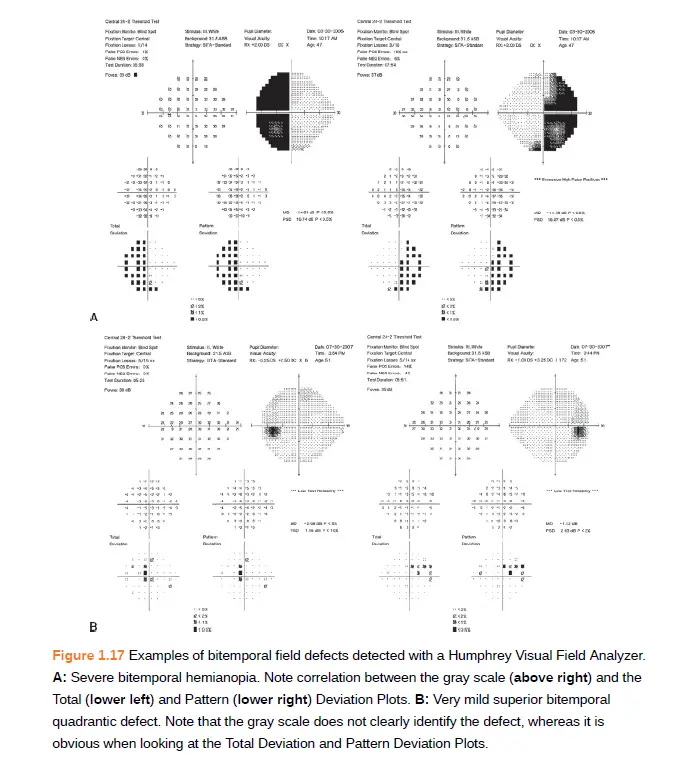
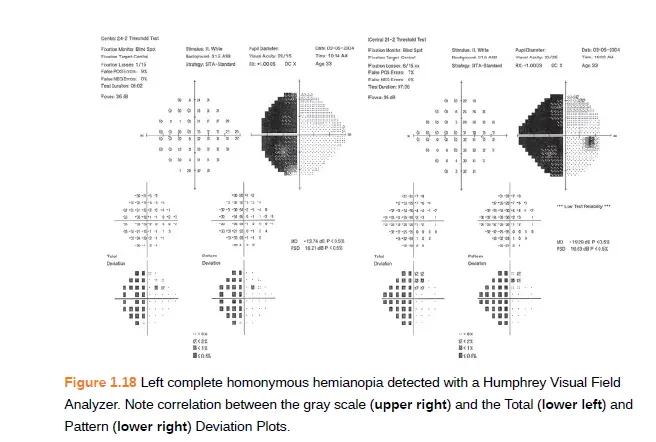
Images taken from book- Walshs and Hoyts clinical neuropthalmology (get from Amazon)
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.