Aberrometry: Essential Tips for Optometrists
Aberrometry has revolutionized the field of optometry by providing detailed measurements of visual aberrations and enabling optometrists to deliver personalized treatments. In this comprehensive guide, we will delve deeper into aberrometry and explore essential tips for optometrists to maximize its potential for accurate diagnosis and optimization of visual outcomes.
Understanding Aberrometry
Aberrometry is a non-invasive technique that measures the refractive errors and aberrations of the eye. It goes beyond conventional methods of diagnosing myopia, hyperopia, and astigmatism, by capturing higher-order aberrations (HOAs). These HOAs include irregularities in the cornea, lens, and other structures of the eye, which impact visual quality. Aberrometry provides a comprehensive analysis of the entire visual system, aiding in the diagnosis of various eye conditions and enabling precise treatment customization.
Ocular wave aberration is a term used to describe the deviations in the optical system of the eye that result in visual aberrations and affect the quality of vision. These aberrations can be categorized into two types: lower-order aberrations (LOAs) and higher-order aberrations (HOAs).
Lower-order aberrations, including myopia (nearsightedness), hyperopia (farsightedness), and astigmatism, are common refractive errors that affect a significant portion of the population. These aberrations can be corrected with traditional glasses, contact lenses, or refractive surgeries like LASIK. While LOAs have a significant impact on visual acuity, they represent only a fraction of the overall aberrations present in the eye.
On the other hand, higher-order aberrations are more complex and encompass a range of irregularities in the optical system beyond standard refractions. These aberrations include coma, trefoil, spherical aberration, and others. HOAs can result from irregularities in the cornea, lens, or other structures of the eye. Unlike LOAs, HOAs are more unique to each individual’s visual system and may not be fully corrected by traditional corrective measures.
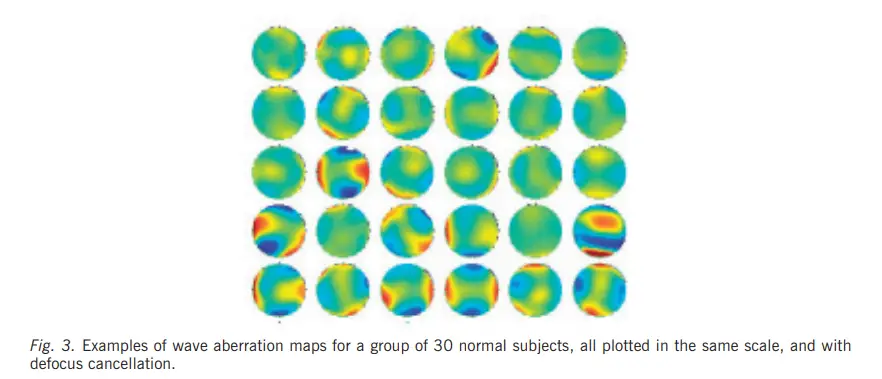
The measurement of these ocular wave aberrations, including both LOAs and HOAs, is accomplished through the use of aberrometers. Aberrometry is a technique that analyzes the wavefront of light as it passes through the eye and provides a detailed analysis of the aberrations present. This measurement is performed using an aberrometer, which captures the wavefront and produces a wavefront map representing the unique pattern of aberrations in the eye.
Aberrometers measure monochromatic aberrations, focusing on a single wavelength of light. Monochromatic aberrations refer to aberrations that occur for a specific color or wavelength of light. By measuring the monochromatic aberrations with an aberrometer, optometrists can obtain a comprehensive understanding of the specific aberrations present in a patient’s eye. This information is crucial for accurate diagnosis and customization of treatment plans.
Tip 1: Patient Preparation:
Proper patient preparation is crucial for accurate aberrometry measurements. It is essential to inform patients about the procedure and provide instructions to remove contact lenses. Soft lens wearers should ideally discontinue lens usage for 24 hours prior to the test, while rigid gas permeable lens wearers may need to abstain for up to a week. This ensures that the cornea returns to its natural shape and prevents lens-induced aberrations that could skew measurement results. Additionally, explaining the procedure to the patient, addressing any concerns, and instilling a sense of comfort and cooperation are important aspects of patient preparation.
Tip 2: Calibration and Alignment:
Accurate calibration and alignment of the aberrometer are critical to obtaining reliable and consistent results. Optometrists must follow the manufacturer’s instructions for calibration to maintain instrument accuracy. Regular calibration checks should be performed to ensure reliable measurements. Equally important is the alignment of the patient’s eye with the device’s optical axis. Proper positioning and fixation on the designated target reduce measurement errors and improve the overall quality of aberrometry readings.
Tip 3: Assessing Higher-Order Aberrations:
Analyzing higher-order aberrations is a significant aspect of aberrometry. These aberrations, such as coma, trefoil, and spherical aberration, can affect visual performance beyond standard refractive errors. Optometrists should familiarize themselves with interpreting wavefront maps and understanding the impact of specific aberrations on visual quality. Through this analysis, optometrists can develop personalized treatment plans that directly address the unique aberrations present in each patient’s visual system. By treating higher-order aberrations in addition to traditional refractive errors, patients can experience improved visual outcomes and enhanced satisfaction.
Tip 4: Multifactorial Analysis:
While aberrometry provides valuable data, it is important to consider other factors that may impact visual quality when making treatment decisions. Evaluating corneal topography, pupil size, and tear film stability alongside aberrometry results offers a comprehensive understanding of each patient’s visual system. Corneal topography aids in identifying irregularities in the corneal structure, which can contribute to aberrations. Pupil size influences the amount of light entering the eye and affects the quality of vision. Tear film stability is essential for maintaining optical clarity. By combining aberrometry with other diagnostic tools, optometrists can optimize treatment outcomes by addressing all relevant aspects that may impact visual quality.
OPTICAL ABERRATIONS OF THE PATHOLOGICAL AND SURGICAL EYE
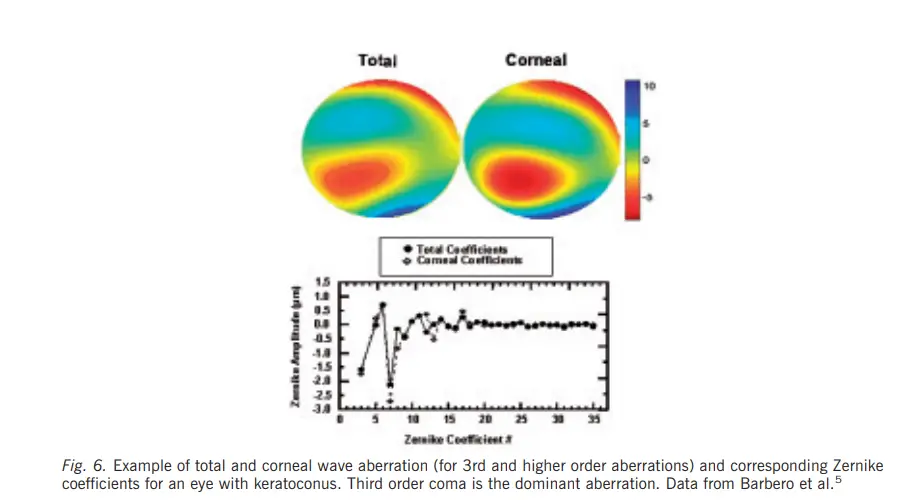
Pathological eyes, due to various eye conditions and diseases, often exhibit abnormal optical aberrations beyond the typical refractive errors. These aberrations can include irregular astigmatism, higher-order aberrations, and changes in the shape and structure of the cornea or lens. For example, corneal irregularities resulting from conditions like keratoconus or corneal scars can introduce irregular astigmatism and higher-order aberrations such as coma or trefoil. These aberrations may cause significant visual distortion and reduced acuity, requiring specific treatment strategies.
Surgical eyes, specifically eyes that have undergone refractive surgeries like LASIK or PRK, can also experience altered optical aberrations. While these surgeries aim to correct refractive errors, they can introduce new aberrations due to tissue removal or reshaping of the cornea. Some common aberrations seen in post-surgical eyes include induced spherical aberration or changes in higher-order aberrations. These aberrations may result in compromised visual quality or night vision symptoms such as glare or halos.
It is essential for optometrists to be aware of the unique optical aberrations associated with pathological and surgical eyes to provide appropriate management and optimization of visual outcomes. Measurement tools like aberrometers are particularly valuable in assessing the precise aberrations present and guiding individualized treatment approaches.
In the case of pathological eyes, specialized contact lenses, such as scleral lenses or custom-designed lenses, can help correct irregular astigmatism and higher-order aberrations, improving visual acuity and quality. In some cases, advanced therapies like corneal cross-linking or corneal transplant may be necessary to address the underlying corneal abnormalities causing aberrations.
For surgical eyes, wavefront-guided or topography-guided ablations can be employed to reduce induced aberrations and improve visual performance. These approaches utilize sophisticated algorithms to customize the laser treatment based on the unique aberration profile of each patient’s eye, aiming for optimal visual outcomes.
In conclusion, pathological and surgical eyes may exhibit optical aberrations beyond typical refractive errors. Pathological eyes can have irregular astigmatism and higher-order aberrations due to various eye conditions. Surgical eyes may experience aberrations induced by refractive surgeries. Understanding these aberrations and employing appropriate management strategies, such as specialized contact lenses or custom ablations, can help optimize visual outcomes in these cases. Regular monitoring and ongoing care are crucial for maintaining good vision in these situations.
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.