Types of Retinal Hemorrhages and its treatment.
What is a retinal hemorrhage?
A retinal hemorrhage occurs when blood vessels in the retina begin to bleed. A hemorrhage, or bleeding, happens when these tiny blood vessels are damaged by injury or disease. Retinal hemorrhage can be caused by diabetes, high blood pressure, head injuries and even sudden changes in air pressure.
Retinal hemorrhages causes
Retinal hemorrhage can stem from various factors, encompassing:
- Medical conditions like hypertension, diabetes, lupus, anemia, infections, and leukemia.
- Ocular disorders, such as macular degeneration, also termed age-related macular degeneration (AMD or ARMD). The macula, situated at the retina’s center, governs our most acute vision.
- Traumatic head injuries arising from accidents.
- Instances of shaken baby syndrome or other forms of child maltreatment.
- Rapid shifts in air pressure during pursuits like mountain climbing or scuba diving, which can reduce retinal oxygen supply.
- Certain medications, notably blood thinners.
- In extremely uncommon scenarios, strenuous activities like severe coughing, vomiting, or constipation.
Types of retinal hemorrhages
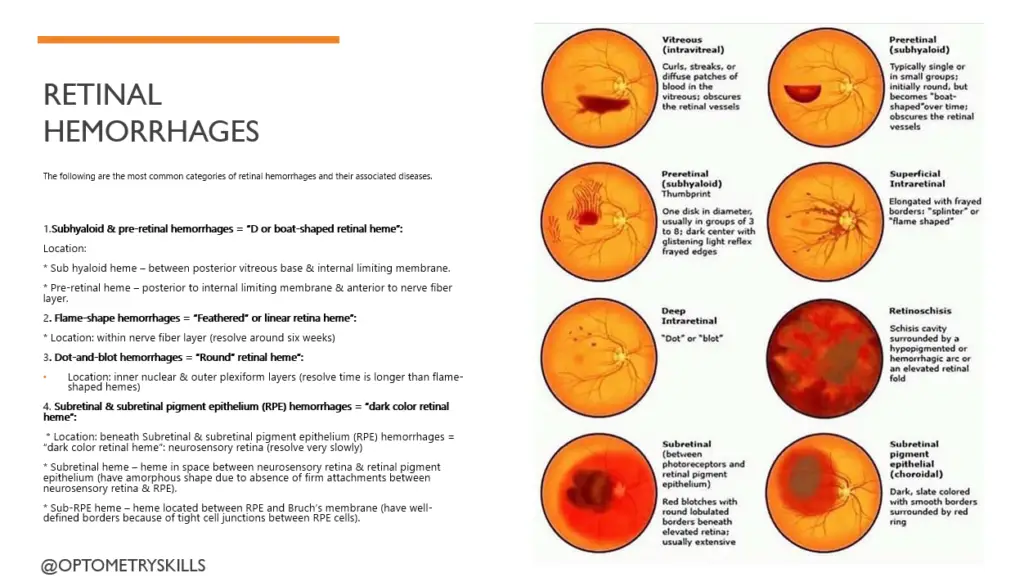
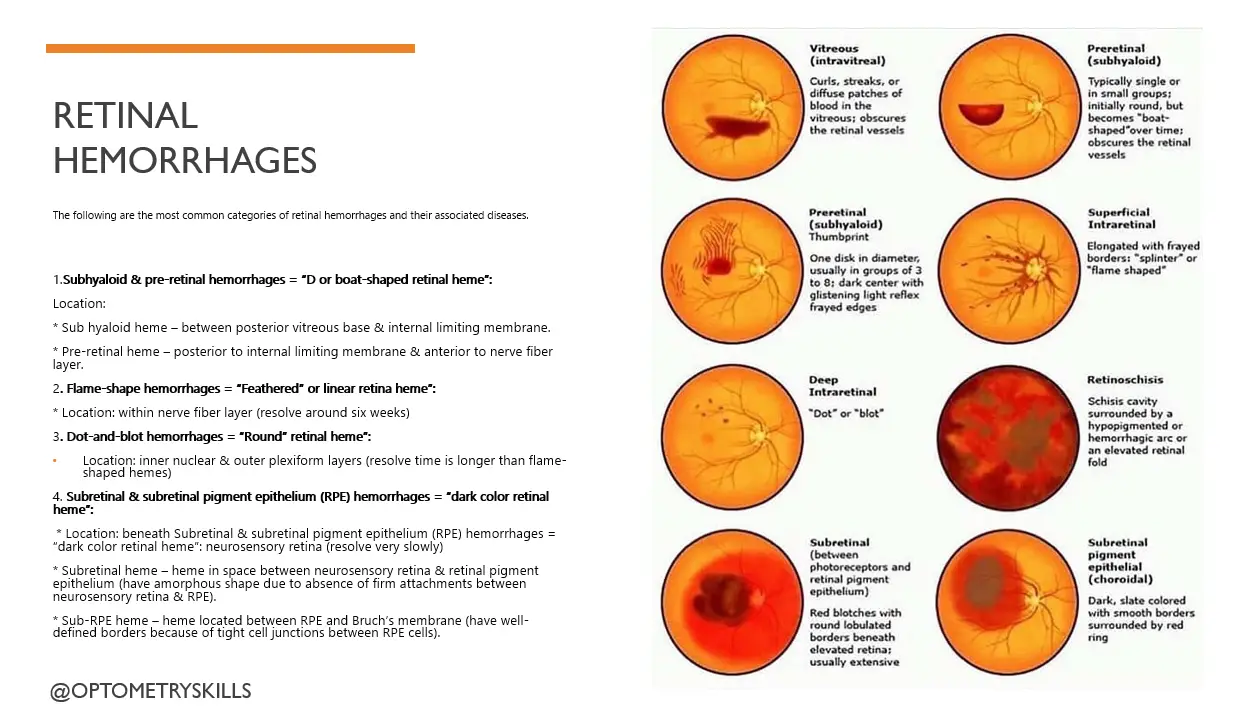
The following are the primary categories of retinal hemorrhages:
- Vitreous and Preretinal Hemorrhages: Blood permeates the vitreous eye membrane, often pooling at the lower eye region. Detectable during eye examinations, these hemorrhages may result from factors like high blood pressure, trauma, or abnormal blood vessel growth linked to conditions such as diabetes. In some cases, the cause remains unidentified.
- Flame-Shaped Hemorrhage: Retinal flame hemorrhages manifest as slender, feather-like, or splinter-like shapes upon eye examination. These hemorrhages are correlated with artery-related ailments like hypertension, blood disorders, and specific forms of anemia.
- Dot or Blot Hemorrhages: Deeper retinal layers host dot or blot hemorrhages, forming circular and uniform patterns. This type can be attributed to factors including diabetes, rare eye or vein disorders, and sickle cell disease.
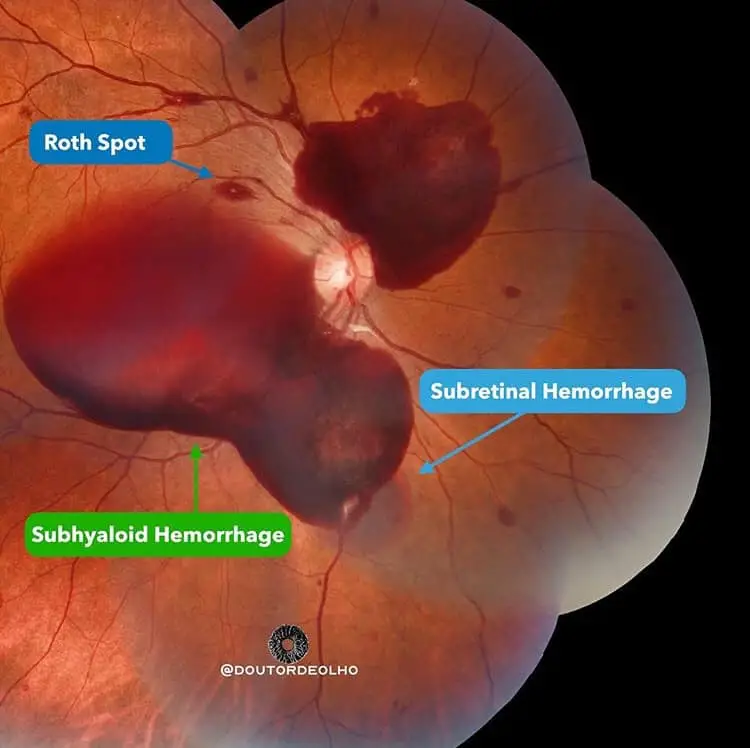
- Roth Spots: A distinctive retinal hemorrhage, Roth spots display a white center. They can signify underlying conditions such as diabetes, leukemia, hypertension, and endocarditis.
- Other Hemorrhage Types: Additional hemorrhage varieties may be linked to conditions like diabetes, hypertension, leukemia, radiation treatments, and various illnesses.
Flame Hemorrhage
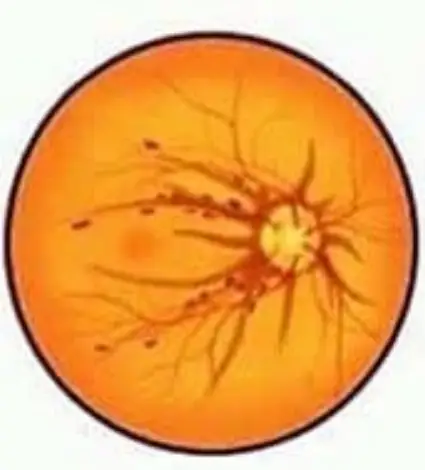
Flame-shape hemorrhages = “Feathered” or linear retina heme”:
* Location: within nerve fiber layer (resolve around six weeks)
* Possible etiologies:
- Hypertensive retinopathy
- Retinal vein occlusions
- Papilledema
- Normal-tension glaucoma
- Anterior ischemic optic neuropathy
Retinal flame hemorrhage, aptly named for their feather-like or splinter-like contours upon eye examination, present a distinctive appearance that is instantly recognizable to ophthalmologists. Their slender and elongated shapes trace along the retinal layers, often emanating from the optic disc or radiating outward. These hemorrhages are usually confined within the nerve fiber layer of the retina, creating an appearance reminiscent of flames.
Etiological Associations: Retinal flame hemorrhage serve as crucial indicators of various systemic and ocular pathologies. Notably, they are strongly correlated with artery-related ailments, thereby offering clinicians essential diagnostic clues.
One of the primary associations lies with hypertension, where elevated blood pressure can lead to the rupture of delicate retinal arterioles, resulting in these distinct hemorrhages. Moreover, specific forms of anemia and blood disorders, such as sickle cell disease, have also been linked to the appearance of flame-shaped hemorrhages.
Dot or blot hemorrhages

Dot-and-blot hemorrhages = “Round” retinal hemorrhages”:
Location: inner nuclear & outer plexiform layers (resolve time is longer than flame-shaped hemes)
Possible etiologies:
- Diabetic retinopathy
- Vein occlusion
- Idiopathic juxtafoveal retinal telangiectasis
- Ocular ischemic syndrome
Dot or blot hemorrhages, characterized by their compact, circular shapes, are embedded within the retinal architecture, often residing in its deeper layers. Their uniform appearance, resembling minute splotches, makes them a distinct pattern discernible to ophthalmologists during retinal examinations. These lesions may arise in clusters, contributing to their distinctive appearance and diagnostic relevance.
Etiological Associations: Understanding the origins of dot or blot hemorrhages requires a comprehensive exploration of potential underlying factors. One prominent association lies with diabetes, where microvascular damage can lead to retinal blood vessel fragility, resulting in these specific hemorrhages. Additionally, these lesions may be attributed to rare eye or vein disorders that compromise vascular integrity. Notably, sickle cell disease, a hereditary condition affecting hemoglobin structure, has also been linked to the appearance of dot or blot hemorrhages.
Subretinal & subretinal pigment epithelium (RPE) hemorrhages
= “dark color retinal hemorrhages”:
Location: beneath neurosensory retina (resolve very slowly)
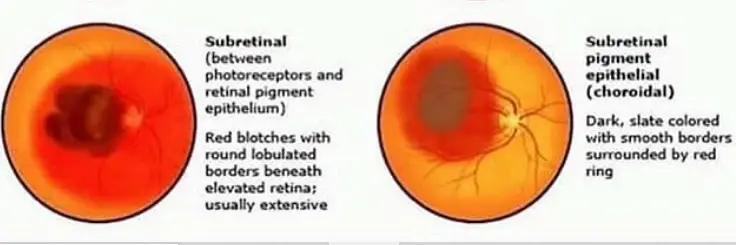
- Subretinal hemorrhages – hemorrhages in space between neurosensory retina & retinal pigment epithelium (have amorphous shape due to absence of firm attachments between neurosensory retina & RPE).
- Sub-RPE hemorrhages – hemorrhages located between RPE and Bruch’s membrane (have well-defined borders because of tight cell junctions between RPE cells).
Possible etiologies:
- Choroidal neovascular membrane formation
- Neurosensory or RPE detachments
- Wet age-related macular degeneration
- Choroidal tumors
- Trauma
Subhyaloid & pre-retinal hemorrhages = “D or boat-shaped retinal heme”:
* Location:
- Subhyaloid hemorrhages – between posterior vitreous base & internal limiting membrane.
- Pre-retinal hemorrhages – posterior to internal limiting membrane & anterior to nerve fiber layer.
* Possible etiologies:
- Retinal neovascularization
- Posterior vitreous detachment & retinal breaks (result of tearing the major retinal vessels)
- Terson’s syndrome (vitreous heme + subarachnoid heme)
- Retinal trauma
- Valsalva retinopathy
Retinal hemorrhages diagnosis
- A dilated eye exam using an instrument called a slit lamp
- Fundus examination
- imaging technique called OCT may be needed
- B-scan ultrasonography
- Intraocular pressure test
- Gonioscopy
Retinal hemorrhages symptoms
- Floaters in Vision: Small, drifting particles within the visual field.
- Appearance of Cobwebs, Streaks, or Lines: Unusual patterns that affect vision.
- Hazy or Blurred Vision: Reduced visual clarity with a sense of haziness.
- Vision with a Red Tint: Visual perception characterized by a reddish hue.
- Worsening Vision in the Morning: Visual deterioration that is more pronounced during morning hours.
When to see the Doctor:
It’s crucial to seek medical attention promptly if you observe any alterations in your eyesight or vision. Reach out to your healthcare provider or an eye care specialist without delay.
In the event that you experience any of the subsequent symptoms, consider heading to the emergency room (ER):
- Sudden Loss of Vision: If you encounter a rapid and unexpected loss of vision.
- Severe Eye Pain: Intense and severe pain in your eyes.
- New Flashes or Floaters: The appearance of new flashes of light or floaters in your visual field.
Do retinal hemorrhages need treatment?
How a retinal hemorrhage is treated depends on a few factors:
- What caused it.
- How much your vision is affected.
- How severe the bleeding in your retina is.
In some cases, the hemorrhage is small and can be monitored while it heals on its own over a period of weeks or months.
If you do need treatment, you might need one of the following procedures:
- Laser or cryotherapy to repair the retinal hemorrhage.
- Vitrectomy: This is the removal of some or all of the vitreous from the middle portion of the eye.
- Intravitreal injection: This involves directly injecting medication into the vitreous.
- Cryotherapy: This involves freezing the retina back into its proper position following a hemorrhage. It can also effectively stop bleeding.
- Laser photocoagulation: This type of eye surgery is used to destroy or shrink abnormalities in the retina.
- An injection of medication like anti-vascular endothelial growth factor (anti-VEGF) or a corticosteroid to reduce inflammation inside your eye.
Risk Factors
The following factors can increase your risk of experiencing a retinal hemorrhage:
- Retinal vascular disease
- Diabetes
- Anemia
- Posterior vitreous attachment
- Normal-tension glaucoma
- Hypertension
- Optic neuropathy
- Primary open-angle glaucoma
Reference: Photo credit: Doutordeolho & aaoeye.
References
- Preventing Recurrent Vitreous Hemorrhage. (December 2006). Ophthalmology.
- Retinal Hemorrhage. (2016). Forensic Epidemiology.
- Retinal Hemorrhage. (August 2022). StatPearls.
- Risk Factors Associated With Retinal Hemorrhage n Suspected Abusive Head Trauma. (April 2015). Journal of the American Association for Pediatric Ophthalmology.
- Retinal Hemorrhages in Shaken Baby Syndrome. (April 2019). The Journal of Pediatrics.
- Retinal Cryotherapy in Diabetic Vitreous Hemorrhage. (2013). Sudanese Journal of Ophthalmology.
- Ophthalmology-Notes And Synopses
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.

You must be logged in to post a comment.