Conjunctival Papilloma
Conjunctival papilloma is a benign squamous epithelial tumor that appears as a fleshy, lobulated, or cauliflower-like mass on the conjunctiva. It may be pedunculated (with a stalk) or sessile (broad-based), and its origin is closely linked to human papillomavirus (HPV) infection, most commonly types 6 and 11.
In addition to viral causes, UV radiation exposure is a contributing factor, especially in limbal lesions in older patients. Papillomas can be solitary or multiple and are often associated with autoinoculation due to eye rubbing or poor hygiene, especially in children.
2. Epidemiology
Seen in both children and adults, with a higher incidence in young adults aged 21–40. There is a slight male predominance. More common in tropical regions and in individuals with frequent outdoor exposure. HPV infection is a key cause, particularly in recurrent or multifocal lesions.
3. Clinical Features
Appearance
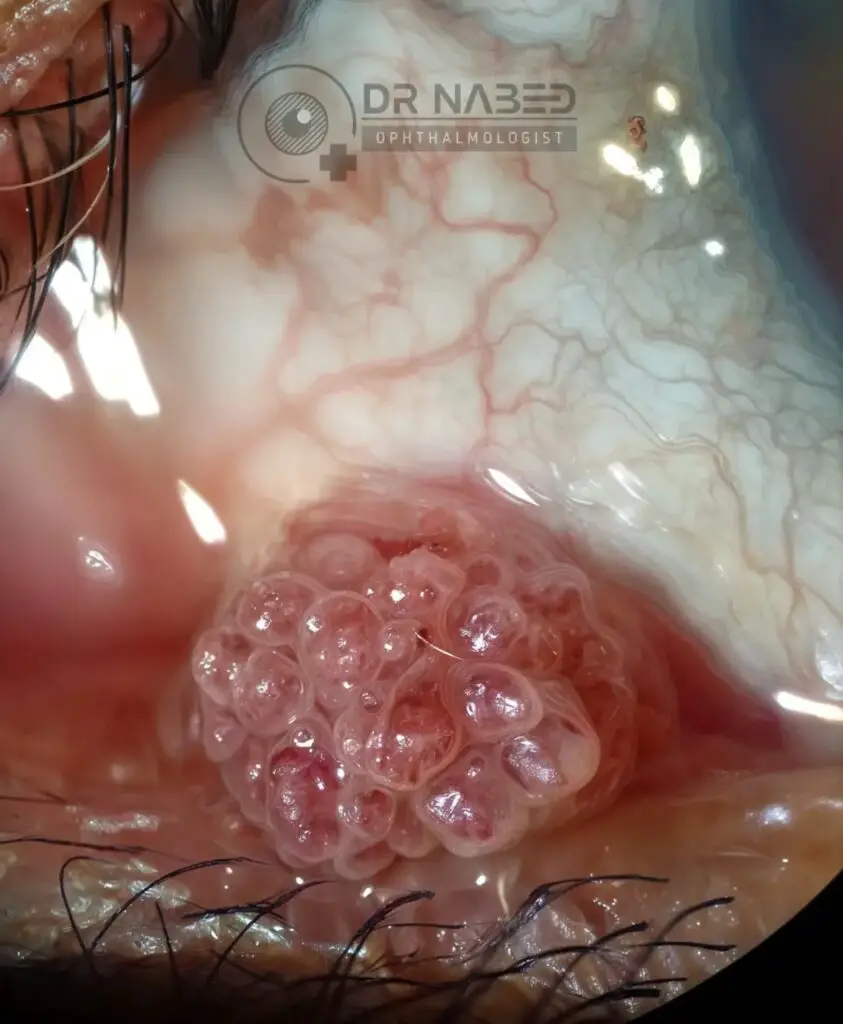
Color: Pinkish-red or grey-white Texture: Lobulated, gelatinous, or papilliform Surface: May be smooth or irregular with visible central vascular cores
Types by Location and Shape
Pedunculated papillomas: Associated with viral etiology, commonly arise from the caruncle, fornix, or palpebral conjunctiva. Sessile papillomas: Common at the limbus; these may be UV-related and have a firmer, broader base.
Common Locations
Caruncle (most frequent site) Palpebral conjunctiva Bulbar conjunctiva Limbus Fornix
Symptoms
Often asymptomatic Irritation or foreign body sensation Tearing Redness Cosmetic concern Rarely, visual disturbance if the lesion encroaches on the cornea
Management
A. Observation
Small, asymptomatic, and non-progressive lesions may be observed with regular follow-up.
B. Surgical Excision
Indicated in cases with visual disturbance, growth, cosmetic concerns, or suspicion of malignancy. “No-touch” technique is preferred to avoid viral spread. Cryotherapy is applied to the base post-excision to reduce recurrence. Complete excision is vital to minimize regrowth.
C. Medical & Adjunctive Therapies
Topical Interferon Alpha-2b: Effective for smaller or recurrent lesions. Topical Mitomycin-C: An antimetabolite used in selected resistant cases. Oral Cimetidine: Has immunomodulatory properties. Laser Therapy (e.g., CO₂ laser): Occasionally used for superficial lesions. Intralesional therapies (e.g., Bevacizumab) have been tried in some recurrences.
7. Prognosis & Recurrence
Recurrence rates vary between 5–30%, especially with incomplete excision or absence of cryotherapy. Malignant transformation is rare but possible, especially in older patients or lesions with atypical histological features. Long-term follow-up is recommended in recurrent cases.
8. Prevention & Patient Education
Hand hygiene is essential to prevent autoinoculation. Advise against eye rubbing, especially in children. UV protection (e.g., sunglasses, hats) helps reduce limbal lesion risk. HPV vaccination may play a preventive role, though ocular-specific evidence is still limited.
Etiology
HPV types 6 & 11; UV exposure
Appearance
Lobulated, pedunculated or sessile mass
Diagnosis
Slit lamp, OCT, biopsy
Management
Excision + cryotherapy; topical antivirals in some cases
Recurrence
Up to 30%; more in limbal or large lesions
References from Standard Ophthalmology Textbooks
Kanski & Bowling, Clinical Ophthalmology: A Systematic Approach – Chapter on Ocular Surface Lesions Albert & Jakobiec, Principles and Practice of Ophthalmology – Tumors of the Conjunctiva Shields & Shields, Tumors of the Conjunctiva and Cornea Yanoff & Duker, Ophthalmology – Ocular Surface Tumors Taylor and Hoyt’s Pediatric Ophthalmology and Strabismus – Viral Eye Diseases in Children
Discover more from An Eye Care Blog
Subscribe to get the latest posts sent to your email.


You must be logged in to post a comment.